Tuberculosis (TB) isn’t very common in the US, but worldwide it causes an immense amount of suffering.
“It’s a persistent, decades-long pandemic,” says Michael Glickman, an infectious disease specialist at Memorial Sloan Kettering and member of the Immunology Program in the Sloan Kettering Institute. “The disease takes its biggest toll in Africa, Asia, and India. Historically, it has been the deadliest infectious killer in the world.”
Dr. Glickman and his colleagues have long been interested in understanding how Mycobacterium tuberculosis, the bacterium that causes TB, infects humans. In 2005, they discovered a “virulence factor” — a particular protein — that the microbe relies on to thwart our immune defenses. Since then, they have been trying to decipher the underlying mechanism of how this virulence factor works. After more than 15 years of hard work, they have finally succeeded.
In a paper published in May 2021 in the journal eLife, Dr. Glickman and his colleagues describe a novel detection system, connected to this virulence factor, that the bacterium uses to sense and counteract our immune defenses. The discovery represents a major advance in scientists’ understanding of how TB thrives in humans, and it gives drug developers a potential new target.
A Sneaky Pathogen
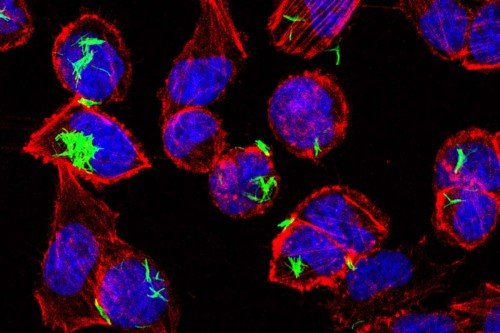
TB spreads when an infected person coughs and sends aerosolized bacteria into the air. Someone else breathes in those bacteria, which land in the lungs. M. tuberculosis is an intracellular pathogen, which means it enters and lives inside cells. It gets some help in this regard from immune cells called macrophages that live in the air sacks of the lungs. Macrophages actively ingest the bacteria and release a toxic payload to try to kill them.
But M. tuberculosis has a variety of sneaky ways to protect itself from the weapons of macrophages. So rather than be killed, it sets up shop in the macrophages and lives — vampire like — off its host.
“TB is trying to have a symbiotic relationship with its human host,” Dr. Glickman says. “In that sense, it’s very different from other more aggressive lung pathogens, which are more immediately fatal.”
The vast majority of adults who become infected with TB are asymptomatic: the microbe multiplies in the body but causes no symptoms. In these people, the immune system is extremely successful at controlling growth of the bacteria, but not eliminating it completely. They have what’s called latent TB, which can persist in the body for decades and reactivate at a later date.
The slow, wasting away that characterizes an active TB infection is why it was once called “consumption”: People seemed to be slowly consumed by it. Consumption was a staple of Victorian literature and opera — Mimi in Puccini’s La Bohème dies from it, for example.
What enables M. tuberculosis to ensconce itself in the lungs and persist for such long periods is the suite of defensive tricks it deploys to defuse macrophage weapons — among them a toxic mix of copper, zinc, and nitric oxide. By resisting or neutralizing these toxins, the bacterium avoids destruction, but the mechanisms by which TB senses and neutralizes these toxins was not understood. And that is where Dr. Glickman’s team made an important discovery.
“Our studies identified an integrated signaling circuit that M. tuberculosis uses to directly sense the combination of stresses that they encounter in the host,” Dr. Glickman says. “When metals like copper and zinc or nitric oxide are detected, the bacteria alter their gene expression to defend against these toxins.”
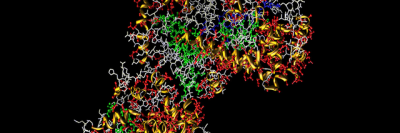
The virulence factor they previously discovered, Rip1, sits at the center of this circuit, and is coupled to another signaling protein, a kinase. Kinases are proteins that transfer chemicals called phosphate groups from ATP, cell’s energy currency, to other proteins; they are a common element of on-off switches in cells.
Biochemically, the signaling circuit the bacteria use to sense and avoid stresses shares similarities with signals that cancer cells use to sense and adapt to the stresses they encounter when forming a tumor. That’s one reason why the Sloan Kettering Institute supports this research, which may have broad lessons applicable to many diseases.
The Other Pandemic
As devastating as the COVID-19 pandemic has been, TB has caused only slightly fewer deaths worldwide every year for the past 100 years.
“People in the US don’t realize how massive a global health problem TB is,” Dr. Glickman says. “It’s ‘out of sight, out of mind.’ ”
TB also doesn’t generate the urgency of something like COVID-19 because it tends to kill people very slowly.
“Nevertheless,” Dr. Glickman adds, “if the COVID pandemic has taught us anything, it’s that infectious diseases don’t respect borders. We are part of a world community, and our research efforts need to seek to understand all the ways in which pathogens can cause disease, as this broad understanding will help us counteract future infectious threats.”