An investigational cancer drug with roots in the Malaysian rainforest is attracting attention as a potential treatment for COVID-19, scientists reported in the February issue of the journal Antiviral Research.
The drug’s anticancer properties have been studied in the laboratory of Hans-Guido Wendel, a physician-scientist in the Cancer Biology and Genetics Program at the Sloan Kettering Institute. Dr. Wendel and collaborators from Germany have now shown that the drug is extremely effective at stopping the replication of SARS-CoV-2, the virus that causes COVID-19.
The drug, called CR-31-B, belongs to a family of chemicals called rocaglates. It is chemically similar to a naturally occurring compound called silvestrol, which comes from the bark of a tree found in the Malaysian rainforest.
“Trees don’t get cancer, but they do struggle with parasitic and viral infections,” Dr. Wendel says. “The antiviral activity of rocaglates may be closer to their original evolutionary purpose.” In other words, fighting infections may be why these chemicals evolved in the first place.
The scientists conducted their experiments in cells growing in a dish. They are now testing the drug in animals with COVID-19 infection.
From Ebola to COVID-19
Dr. Wendel began collaborating with Arnold Grünweller and his team at the University of Marburg during the Ebola outbreaks in the Congo in 2014. They wondered if CR-31-B would have activity against Ebola. Indeed, they found that the compound was active against Ebola as well as several different families of RNA viruses, including coronaviruses such as SARS and MERS.
The amount of CR-31-B needed to clobber these viruses was miniscule and was not toxic to the infected cells. The German team published these results earlier this year in the journal Antiviral Research.
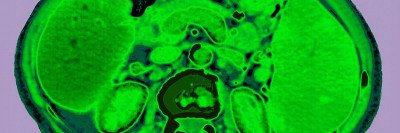
The team has now shown that CR-31-B can also beat back SARS-CoV-2 with similarly small amounts. They tested different amounts of the drug in both monkey and human cells growing in a dish and found that it blocked the virus at doses that were not toxic to the cells.
The scientists also compared the effectiveness of CR-31-B to the drugs chloroquine and remdesivir, which have both been explored as possible treatments for COVID-19.
“Chloroquine doesn’t do anything, and remdesivir is about 100 times less effective than this drug,” Dr. Wendel says.
How It Works
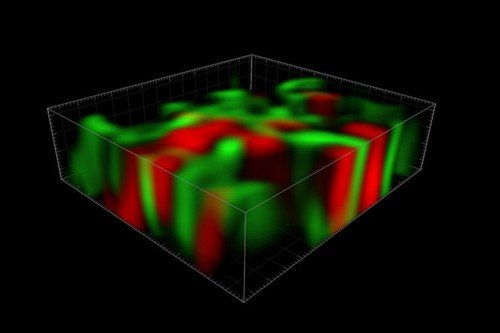
From studying rocaglates in the lab, Dr. Wendel has learned that they work by blocking an enzyme called RNA helicase found in cells. This enzyme allows messenger RNAs (mRNA) with complicated structures to be made (technically, translated) into protein.
One such complicated mRNA is that of the oncogene MYC, which drives cancer cells to proliferate. Without working helicase, the cancer cells’ ability to translate the MYC mRNA into the MYC protein is prohibited and so they die.
Silvestrol and related compounds show remarkable efficacy in treating several types of cancer in mice, including leukemia and lymphoma. Silvestrol itself is hard to extract from its source tree in large amounts, and its complicated chemical structure makes it hard to create from scratch, so Dr. Wendel’s lab has collaborated with the Tri-Institutional Drug Discovery Initiative (Tri-I-TDI) to make simpler synthetic versions. Studies are ongoing to develop these drugs for testing in clinical trials for people with cancer.
Resisting Resistance
What’s particularly interesting about rocaglates in comparison with other antiviral drugs is that they don’t target viruses directly. Rather, they target an enzyme in the cell the virus infects — that is, a host enzyme. This is potentially a boon for medicine, since viruses mutate quickly and can evolve resistance to drugs that directly target them. This is what can happen with the antiviral drug remdesivir, for example. Since viruses have no control over host enzymes, however, they cannot develop resistance as easily to drugs directed at these enzymes.
“That’s a big deal and a relatively new idea,” Dr. Wendel says.
A potential drawback of targeting host enzymes is the potential for toxicity or side effects. But from the team’s earlier work investigating rocaglates in the context of cancer, they know that these compounds are well tolerated — at least by mice.
The rocaglate work has already attracted attention from eminent virologists in the research community, including David Ho at Columbia who developed some of the first effective HIV drugs, and other labs around the world that are involved in testing too.
Dr. Wendel had previously tried to interest pharmaceutical scientists in the antiviral activity of rocaglates in the pre-COVID-19 era. “Nobody was interested in antivirals back then,” he says. Now, he says, things look very different.