Some cancer treatments — including bone marrow transplantation, chemotherapy, and radiation — can temporarily deplete the body of infection-fighting white blood cells called T cells, leaving patients vulnerable to infections.
Now Memorial Sloan Kettering researchers have shed light on a biological process that allows T cells to regenerate naturally after such therapies. Published in the April 6 issue of the journal Science, their findings from studies conducted in mice hold hope for the development of a new type of drug that would allow people to regain their immune defenses more quickly.
“This natural process could potentially be harnessed to treat different forms of T cell deficiency caused by cancer treatments, radiation injury, infections, or autoimmune diseases,” says clinician-scientist Marcel R. M. van den Brink, head of Memorial Sloan Kettering’s Division of Hematologic Oncology and a member of the Sloan Kettering Institute Immunology Program, who led the research.
Restoring the Thymus
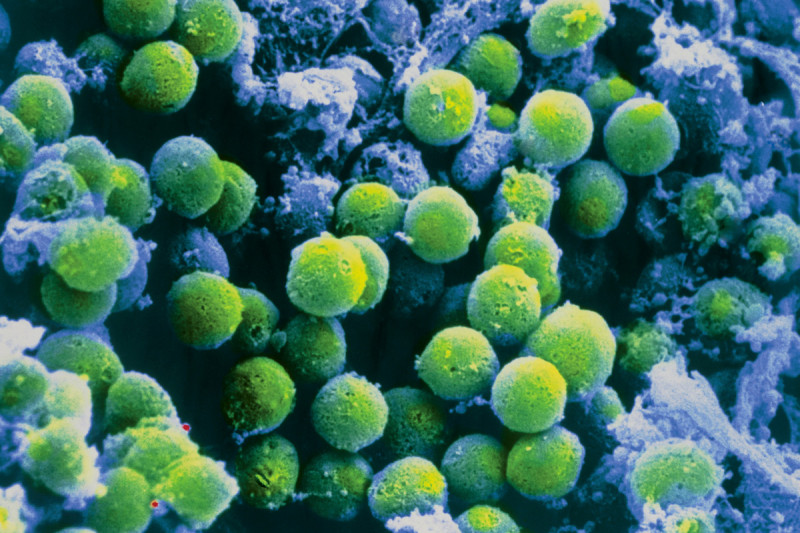
T cells, which defend the body from infection by intruders such as viruses, bacteria, and fungi, undergo part of their development in the thymus, a small organ situated underneath the breastbone.
“The thymus is very sensitive to damage,” explains Sloan Kettering Institute postdoctoral fellow Jarrod Dudakov, the first author of the Science report. “For example, when a person is exposed to radiation or toxic chemicals, the function of the thymus is easily impaired, ultimately leading to reduced levels of mature T cells and an increased risk of infection.”
When not doing laboratory research, Dr. van den Brink specializes in treating patients with certain cancers and blood disorders using allogeneic bone marrow transplantation, in which patients receive blood-forming stem cells from a donor. He adds that this procedure can severely weaken the thymus, often increasing a patient’s risk of getting a life-threatening infection for one year or longer.
“However,” he says, “the thymus has the remarkable capacity to rebound and start generating new T cells over time — especially in people who are young and healthy.”
To better understand how the thymus regenerates, Drs. van den Brink, Dudakov, and their colleagues examined the thymus following immune injury and revealed a network of molecular mechanisms that triggers different cell types in the thymus to rejuvenate. Their research suggests that a protein called IL-22 — secreted by cells in the thymus called lymphoid tissue inducer cells — can promote the regeneration of a weakened thymus.
The investigators induced thymic damage in mice, and demonstrated that an injection of IL-22 protein sped up the recovery of T cells.
“Our results suggest it might be possible to use IL-22 in a clinical setting to give the immune system a boost,” Dr. van den Brink says, while noting that additional research needs to be done to confirm that this strategy could be beneficial for humans.
A Variety of Potential Applications
“Occasionally, my colleagues and I lose patients who have undergone lifesaving transplants due to infection-related complications,” Dr. van den Brink says. “It is devastating to watch this happen, knowing we could have potentially prevented infection if there was a way to strengthen the thymus and speed the recovery of T cells.”
While no such treatment currently exists, a prospective drug for regenerating T cells could make it possible to treat T cell deficiency in a number of additional settings — for example, in people whose thymic function has been impaired by HIV/AIDS, autoimmune disorders, malnutrition, or radiation poisoning due to a nuclear disaster. It also holds promise as a vaccine adjuvant — a type of therapy used to augment the effectiveness of vaccination — for people with weak thymic function.
“Because the thymus naturally deteriorates with age, there is a great medical need for such therapies for elderly people,” Dr. van den Brink explains. For example, nine out of ten deaths from flu viruses occur in people who are 65 and older.
The investigators are now conducting studies in the laboratory to assess the potential of IL-22 for several clinical applications, including allogeneic bone marrow transplantation and vaccination.