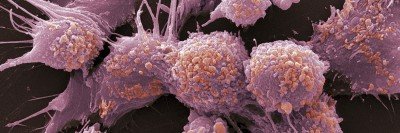
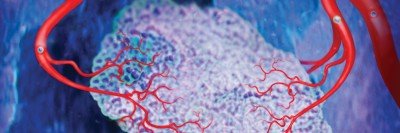
Cancer doesn’t exist on its own within the body. It thrives within what is called the tumor microenvironment — the ecosystem of tissues, blood vessels, immune cells, and noncancerous components surrounding a tumor. More and more research is focusing on understanding the tumor microenvironment because it could lead to new ways to treat cancer.
A team of doctors and researchers from Memorial Sloan Kettering is reporting that they’ve found a protein within the microenvironment of certain prostate cancers that empowers the tumors to resist therapy. Now that that they’ve found this protein, they believe they may be able to block it and prevent therapy resistance. The study was published online July 16 in Cancer Cell.
“We’ve done a lot of research on prostate cancer over the past ten years, but most of the focus has been on molecular changes within the tumor cells themselves,” says physician-scientist Charles Sawyers, Chair of MSK’s Human Oncology and Pathogenesis Program and the paper’s senior author. “Until now, looking at the microenvironment as a cause of resistance to treatment hasn’t really been on our radar.”
Finding a Way around Drug Resistance
Treatment for prostate cancer is personalized depending on whether the tumor has spread and its grade (how likely it is to spread in the future). Early-stage, low-grade disease can usually be successfully treated with surgery or radiation therapy. For men with high-grade tumors that have spread beyond the prostate but not to other parts of the body (called locally advanced), the standard treatment is either surgery or radiation, often combined with a drug treatment called androgen deprivation therapy (ADT).
ADT blocks testosterone and other male hormones that prostate tumors need to grow and survive. The problem is that many tumors eventually find a way around this obstruction and start feeding on these hormones again.
Over the past several years, Dr. Sawyers and others have led the development of new drugs that help restore sensitivity to androgen blocking. But this, too, has proven to be only a temporary fix: Many tumors eventually are able to start growing again. There remains a need to develop new approaches.
In men with high-grade, locally advanced prostate cancer, the disease comes back in about 60% of patients, according to surgeon Brett Carver, a member of Dr. Sawyers’ lab who co-authored the paper. “This new research shows that resistance to treatment isn’t coming only from the tumor itself; it may also be caused by some aspect of the microenvironment,” Dr. Carver says.
Connecting Lab Research to Patient Samples
Because the tumor microenvironment has proven to be important in other cancers, Zeda Zhang, the paper’s first author and a Gerstner Sloan Kettering student working in Dr. Sawyers’ lab, decided to study the role of the microenvironment in prostate cancer. The research in this paper focused in particular on studying locally advanced tumors treated with ADT.
In mouse models and cell cultures of prostate cancer, they found that a protein called NRG1 is elevated in a type of cell that surrounds prostate tumors, called stromal cells. NRG1 activates another protein called HER3, which allows cancer cells to get around the hormone blockade and drives tumor growth.
“When tumor samples from patients who had received androgen deprivation therapy and those who had not were studied, the results were as expected,” says medical oncologist Dana Rathkopf, another co-author on the paper. “Some of the men who received androgen deprivation therapy also had increased levels of NRG1.”
Developing Drugs for Different Targets
HER3 and a related protein called HER2 are common targets for cancer therapy, especially in breast cancer. But so far, HER2- and HER3-blocking drugs have been disappointing in treating prostate cancer. Dr. Sawyers says it may be possible to develop a treatment such as an antibody that would block these proteins in a different way than what’s been tried before. “It’s compelling because there are already such antibodies in development for other conditions,” he says.
Dr. Carver adds that one particular experimental antibody used in the lab has already shown that this approach is likely to be successful. The researchers reported this finding in the paper.
“One of the strengths of doing research at MSK is the flow of information between lab scientists and doctors in the clinic,” Dr. Rathkopf concludes. “It gives us a more complete picture of what’s happening, which can help us make treatment decisions in real time and improve outcomes for those in need of new therapies.”
This work was funded by National Institutes of Health grants R01 CA155169–04, R01 CA19387-01, R01 CA166413, R01 CA204232, R00 CA218885-04, P30 CA008748, U54 OD020355, P50 CA092629-14, P30 CA008748-49, P3 CA008748-49-S2, 1R01 MH117406, and P30 CA008748; the Howard Hughes Medical Institute, the Starr Cancer Consortium, the Department of Defense, the Cancer Prevention and Research Institute of Texas, the Vallee Foundation, the Prostate Cancer Foundation, the Dutch Cancer Foundation, the Welch Foundation, the WorldQuant Foundation, the Pershing Square Sohn Cancer Research Alliance, a University of Texas Southwestern (UTSW) Deborah and W.A. Tex Moncrief, Jr., scholarship, and a UTSW Harold C. Simmons Cancer Center Pilot Award. Zeda Zhang is supported by a National Cancer Institute Predoctoral to Postdoctoral Fellow F99/K00 Transition Award.
Charles Sawyers is a co-inventor of enzalutamide and apalutamide and may be entitled to royalties. He also serves on the Board of Directors of Novartis and is a co-founder of ORIC Pharmaceuticals. He is a science advisor to Agios, Beigene, Blueprint, Column Group, Foghorn, Housey Pharma, Nextech, KSQ, Petra, and PMV. Dana Rathkopf has had uncompensated consulting or advisory roles with Genentech/Roche, Janssen Oncology, and TRACON Pharma. She has received research funding from AstraZeneca, Celgene, Ferring, Genentech/Roche, Janssen Oncology, Medivation/Astellas/Pfizer, Millennium, Novartis, Taiho Pharmaceutical, Takeda, and TRACON Pharma for her work at MSK.