To an immunologist, autoimmune diseases like Type 1 diabetes are the polar opposite of cancer. In the former, the immune system goes into overdrive and attacks the body’s own organs in a relentless manner, eventually causing disease; with cancer, the immune system shuts down and fails to mount an aggressive attack to stop cancer from forming.
Why does the immune system behave so differently in the two cases? No one knows.
“This is a real mystery in the field,” says Andrea Schietinger, a tumor immunologist in the Sloan Kettering Institute (SKI) at Memorial Sloan Kettering Cancer Center who studies the phenomenon of immune cell dysfunction in cancer.
“We thought if we could figure out how autoimmune T cells are programmed, then we could take that information and apply it to tumor-specific T cells to make them more effective cancer killers.”
It was a bit of a long shot. To pursue this ambitious research project, Dr. Schietinger was awarded a National Institutes of Health (NIH) Director’s New Innovator Award in 2017, a funding opportunity that specifically supports high-risk, high-reward science. The project became a collaborative effort between Dr. Schietinger’s research team, particularly Sofia Vaccarino Gearty, an MD/PhD student in the lab, and scientists Doron Betel, Friederike Dündar, and Paul Zumbo from Weill Cornell Medicine.
Now, four years later, the results are in. Researchers reported in the journal Nature, on November 30, 2021, that the ability of autoimmune T cells to continue fighting is dependent upon a population of stem-like T cells that perpetually resupply the stock of self-reactive T cells. This type of stem-like T cell has never been seen before in autoimmune diseases, and the researchers think it could hold important lessons for improving the treatment of both autoimmune diseases and cancer.
Modeling Diabetes in Mice
Type 1 diabetes is caused when the body starts making T cells that specifically recognize and kill the insulin-producing cells of the pancreas. These are called beta cells. When 80% or more of the beta cells are killed, the body can no longer regulate the level of glucose in the blood and diabetes results.
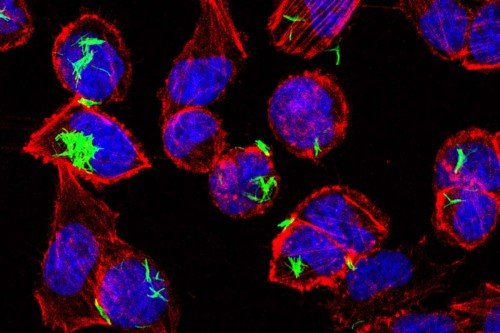
To explore what makes Type 1 diabetes unique, the researchers turned to a mouse model of the disease that closely mirrors what happens in people with the disease. They used a technique to label the “killer” (CD8) T cells that recognize and kill the beta cells. This allowed the researchers to see where the T cells were coming from and where they were going. Then, the team followed these T cells for more than 30 weeks in the mice.
Like all immune cells, CD8 T cells travel through the body in lymphatic vessels that periodically intersect with lymph nodes that serve as “depots,” where immune cells meet telltale markers (called antigens) from potential threats like microbes or cancer. From these lymph nodes, T cells then travel into tissues, where they go on the attack. In the case of autoreactive T cells in diabetes, the cells travel from a lymph node near the pancreas into the pancreas itself, where they find and kill the beta cells.
By closely studying these cells along their journey, the researchers were able to see that the T cells in the lymph node had some unique properties compared with those that ended up in the pancreas. In particular, the T cells in the lymph node had markers suggesting they were stem cells. The T cells in the pancreas did not have these markers.
The researchers noted other curiosities. The T cells didn’t last very long in the pancreas. Rather, they killed a few beta cells and then they themselves died. But a fresh crop of autoreactive T cells continually arrived in the pancreas to replace those that died.
To the scientists, this suggested that the T cells in the lymph node serve as stem cells that continue to regenerate the supply of self-reactive T cells in the pancreas. And it provided an answer to the longstanding puzzle of why autoreactive T cells don’t get exhausted in the same way tumor-specific T cells do: They are continually being replaced.
In fact, it’s the perpetual replacement of self-reactive T cells that constitutes the autoimmune disease of diabetes; if the T cells weren’t replaced, they would be unable to cause disease because they die too quickly.
Only a Few Cells Necessary to Cause Disease
That’s what appeared to be happening. But to prove the stem cells were responsible for causing disease, the scientists did another experiment. They transferred a handful of these cells to a new mouse and watched to see if the mouse developed diabetes. Sure enough, transferring as few as 10 of the cells was enough to cause diabetes in the mouse. Not only that, but transferring a few of these cells from the newly diabetic mouse to a third mouse was enough to make the new mouse diabetic. And so on and so forth, for more than seven months.
By contrast, transferring hundreds of thousands of the pancreatic T cells to a new mouse could not cause the disease. This told the researchers that the stem-like cell population was crucial for causing the disease.
Next, they asked what would happen if T cells were unable to migrate into the pancreas. The researchers knew of a drug that prevents T cells from migrating out of lymph nodes. When the researchers gave this drug to their mice, the mice were protected from diabetes — ostensibly because the dying T cells in the pancreas could not be replaced by new ones. This experiment provided further evidence of the importance of this stem-like cell population in causing disease.
Such a stem-like cell population has never before been implicated in Type 1 diabetes, and Dr. Schietinger thinks that it could be an attribute of other autoimmune diseases as well.
A Special Place for Fundamental Research
Dr. Schietinger never expected to be working on diabetes when she came to SKI six years ago. “I assumed the expectation would be that as a tumor immunologist I would work on cancer only, but that’s not the case,” she says. “SKI has a really strong commitment to supporting fundamental basic science wherever it leads. It’s one of the attributes that makes working here so special.”
She and her team are now collaborating with diabetes specialists at MSK and other institutions to work on the next set of exciting questions.
Ultimately, they hope to be able to treat autoimmune diseases and translate these lessons from diabetes to cancer, to help keep immune cells fighting cancer for longer.
- Autoimmune diseases such as diabetes result when self-reactive immune cells attack the body’s own organs.
- Unlike the situation in cancer, immune cells in autoimmune diseases do not get exhausted and instead keep attacking their targets, which is what makes the conditions so dangerous.
- Researchers at SKI wanted to know what is unique about autoreactive T cells and used a mouse model of diabetes to study these cells.
- They found that a unique population of stem-like cells continually replenishes the self-reactive T cells in diabetes, a finding that has implications for treating both autoimmune diseases and cancer.