The proteins making up CAR T cells can be tweaked to give the cells different properties, like how long they last in the body.
Chimeric antigen receptor (CAR) T cells are genetically engineered human immune cells that are designed to fight cancer. They have shown great promise in treating people with deadly forms of leukemia and lymphoma. Despite this early success, scientists are actively trying to improve the safety and efficacy of these powerful cancer killers.
Researchers at Memorial Sloan Kettering led by immunologist Michel Sadelain reported on December 17 in the journal Nature Medicine that they have found a way to tweak the current CAR model to improve its performance.
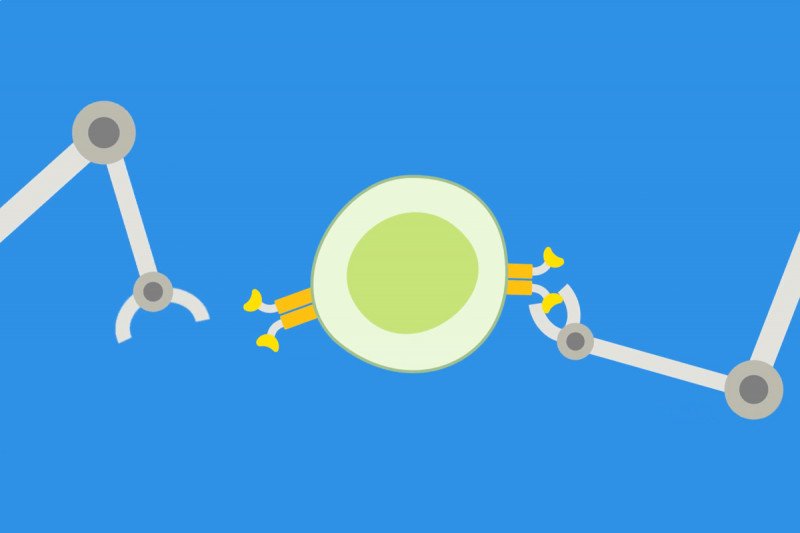
The CAR designs in use today all share a common structure: a region on the outside of the cell that resembles an antibody and an inner region that borrows parts from T cell receptors. To this basic chassis, scientists add one of two different immune gas pedals, CD28 or 41BB, to make what are termed second-generation CARs. When infused into the body, these cells grow and divide as they seek out and fight cancer.
Like natural T cells, CAR T cells must navigate a path between a memory mode and an attack mode — between mounting a full-on assault and sticking around to fight another day. By comparing existing CARs on the clinical racetrack, it’s become clear that CD28 CARs tend to be quicker killers, but they peter out faster than the sluggish yet enduring 41BB CARs.
In their new paper, Dr. Sadelain’s team reports that the persistence of CD28-based CARs can be improved by tweaking the inner domain, specifically a part called CD3zeta. This is the region that initiates the signal to the T cell, in effect telling it to attack. Within CD3zeta, amino acid sequences called ITAMs serve as amplifiers, tuning the intensity of the signal.
Using a mouse model of leukemia, the scientists found that the number of ITAMs present in a CAR played a big part in shaping which path the cell took.
Video: CAR T Cell Therapy: What It Is and How It Works
“Current CAR designs come with three ITAMs,” Dr. Sadelain says. “We found that by varying the number of working ITAMs, we could increase the longevity of the CAR T cells without compromising their tumor-killing power.”
Judith Feucht, a postdoctoral fellow in the lab and one of the paper’s first authors, adds, “We hope that the novel CAR designs with their enhanced therapeutic profiles will not only further increase response rates in people with leukemia but also improve CAR therapy against other cancers.”
The refurbished CARs will soon be tested in clinical trials at MSK.