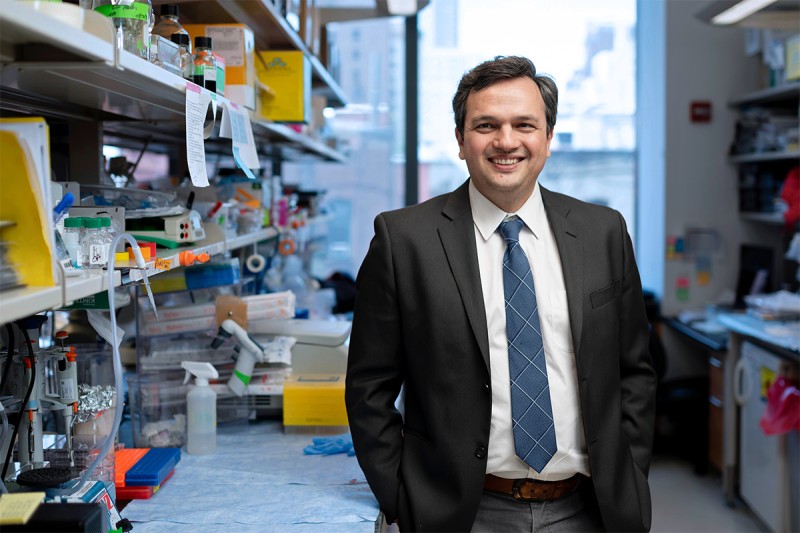
Dr. Piro Lito has spent many years developing drugs to treat cancers caused by KRAS.
KRAS was one of the first cancer genes ever discovered, but for a long time the cancer-causing KRAS protein was considered “undruggable” with targeted therapy. That started to change in May 2021, when the Food and Drug Administration granted accelerated approval to sotorasib (Lumakras®) for lung cancers caused by a particular KRAS mutation, called KRAS G12C. The approval of sotorasib was based on years of lab research and clinical trials, much of that work led by physician-scientist Piro Lito, MD, PhD, and other investigators at Memorial Sloan Kettering Cancer Center (MSK).
But G12C is only one of many mutations in KRAS (pronounced “kay-rass”) known to cause cancer, and lung cancer is only one of many cancers linked to these mutations. In a paper published May 31, 2023, in Nature, investigators led by Dr. Lito reported results for a new molecule that can block many more mutated forms of the KRAS protein. In the lab, the compound was effective at blocking the growth of multiple cancer cell lines, including lung cancer, colon cancer, and pancreatic cancer. It was also effective in mouse models of lung and colorectal cancers caused by KRAS.
“KRAS is one of the most frequently activated proteins in cancer,” says Dr. Lito, a thoracic oncologist who also heads a lab in MSK’s Human Oncology and Pathogenesis Program. “Although they are important, the drugs that we have developed so far only help a limited number of people. The inhibitor described in this paper has key therapeutic implications for treating patients with more types of cancer and more KRAS mutations.”
Compound Inactivates a Range of KRAS-Mutant Proteins
KRAS-driven cancers have long been considered undruggable due to the protein’s uncommon shape. Because KRAS is smooth and round, it was difficult to find a targeted drug that could wedge in and block the protein’s activity. A decade ago, researchers discovered that the G12C version of the protein had a small pocket that opened and closed, depending on whether the protein was active. Within a few years, drugs were developed that could fit into that pocket and switch the protein off. But those drugs were ineffective against other forms of KRAS mutations that didn’t have the pocket.
BI-2865, the inhibitor analyzed in this study, binds to the KRAS protein in a different way, taking advantage of characteristics of the protein that were not previously known.
“We were surprised that BI-2865 was able to inactivate the most frequent cancer-causing KRAS mutants,” says Dongsung Kim, PhD, a research associate with Dr. Lito and the study’s first author. “These mutants were thought to be locked in an active state in cancer, but if that were true this drug would not work at all. This research opens a new direction in our understanding of how these mutations cause cancer.” In fact, studies in the lab showed that the new inhibitor was able to block 15 other versions of KRAS in addition to the G12C mutation.
Moving New KRAS Inhibitors into Clinical Trials
BI-2865 was developed by investigators from the pharmaceutical company Boehringer Ingelheim, who collaborated on this study and co-supervised it. It is a prototype that will need to be refined before testing in patients, but the company is working on new molecules that are optimized for clinical development. Dr. Lito plans to continue working with investigators from the company and hopes to have drugs that could be tested in clinical trials within a year.
“The ability to target multiple KRAS mutants with a single molecule provides more definitive evidence that KRAS is finally druggable after more than 40 years of research,” Dr. Lito says. “This work has the potential to benefit a large number of people with cancer, including lung, colorectal, and pancreatic cancers.”