There is a clear and unmet need for less invasive and more accurate methods for diagnosing lung cancer. A promising innovation under investigation at Memorial Sloan Kettering Cancer Center (MSK) is the electronic nose (e-nose), which evaluates volatile organic compounds (VOCs) in exhaled breath. The e-nose platform detects a lung cancer-associated “breathprint” in breath from individuals with lung cancer.
“E-nose technology has enormous potential for transforming the diagnosis and clinical management of lung cancer, including lowering high false-positive rates seen with imaging, identifying subtypes and genetic mutations, predicting and evaluating treatment responses, and guiding the development of precision treatment strategies,” said MSK thoracic surgeon Gaetano Rocco, MD. “However, more evidence from large, prospective trials of next-generation devices is needed before we can integrate the e-nose into clinical practice.”
Dr. Rocco, thoracic surgery research fellow Stijn Vanstraelen, MD, and thoracic surgeon David Jones, MD, summarized the advantages, disadvantages, diagnostic accuracy, and possible improvements for various e-nose technologies in development in an invited expert opinion published recently in the Journal of Thoracic and Cardiovascular Surgery. (1)
Dr. Rocco and colleagues are now conducting a series of prospective observational trials testing the accuracy of next-generation e-noses at MSK.
Room for Improvement: Current Lung Cancer Diagnostics
Standard diagnostics for lung cancer include a combination of blood tests, computed tomography (CT), and positron emission tomography. (2) (3) (4) (5)
Low-dose CT scans of early-stage tumors can yield high false-positive rates, leading to unnecessary invasive biopsies or surgeries for definitive diagnoses. Further, up to 11% of resected small lung nodules without preoperative pathologic confirmation are benign. (6) (7)
How E-Nose Technology Works
The human breath contains as many as 3,000 VOCs in parts per million, with some present in concentrations as low as parts per trillion. (5) (8) VOCs created by various cellular metabolic pathways are altered in cancer, including cytochrome P450 and oxidative stress, (5) (9) the Warburg effect, (10) (11) and genomic mutations. (5) (12)
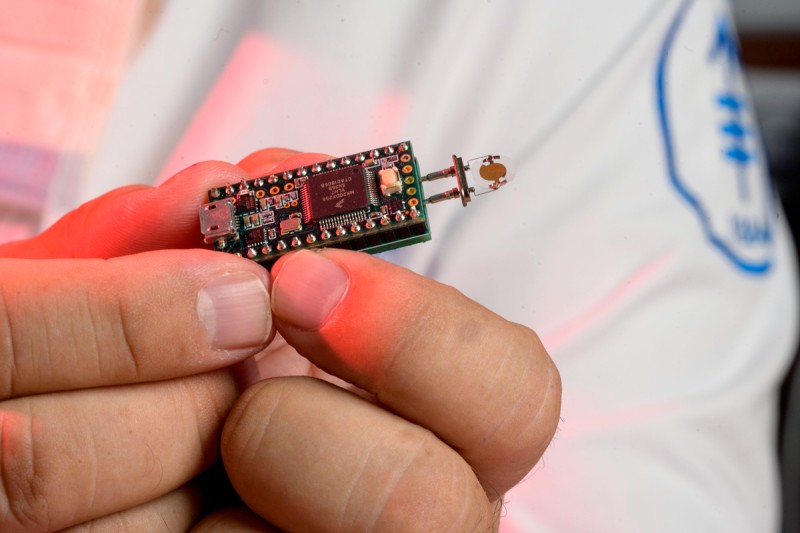
An e-nose device contains an array of electronic chemical sensors connected to a pattern-recognition platform. When VOCs react on the sensors’ surface, changing their conductivity, transducers convert them into electrical signals, creating VOC signatures called breathprints. The breathprints are compared to a large library of VOCs specific to a disease like lung cancer. (1)
There are several different e-nose technologies. For example, the Cyranose 320 uses a carbon black polymer sensor array, whereas the BIONOTE (BIOsensor-based multisensorial system for mimicking NOse, Tongue, and Eyes) platform has quartz crystal microbalance sensors with anthocyanin-coated electrodes. (13) In their op-ed, Dr. Rocco and colleagues provided a table summarizing the advantages, disadvantages, possible improvements, and diagnostic accuracy for 10 different e-nose technologies. (1) They noted several research teams worldwide have found e-nose technology to be highly accurate in distinguishing malignant from benign pulmonary nodules. It has also shown merit in differentiating lung cancer histological subtypes, identifying genomic alterations, and predicting responses to immunotherapy. (1)
Promising First-Generation Evidence
Dr. Rocco has been investigating e-nose technology for the early identification of lung cancer for almost a decade. As a thoracic surgeon at the Istituto Nazionale Tumori, Fondazione Pascale, IRCCS, he and his colleagues evaluated the first-generation BIONOTE platform created at the Campus Biomedico University in Rome, Italy.
Their study found BIONOTE had promising potential for reducing false positive rates compared with low-dose CT: Among 100 individuals screened, BIONOTE demonstrated an overall sensitivity of 86% and specificity of 95%. The cost per breathprint was only €10. The study results were published in the European Journal of Cardio-Thoracic Surgery in 2016. (4)
In their recent opinion editorial, the MSK co-authors wrote that further improvements in detection accuracy and the availability of real-time readouts would be required to increase the potential for incorporating e-nose technology as a complement to existing diagnostic strategies. They also highlighted the need for low-cost and smaller devices. (1)
Research Underway at MSK
Dr. Rocco and colleagues are now investigating next-generation e-noses in a series of prospective observational trials. Based on the BIONOTE technology, these newer devices provide substantially faster processing times and real-time readouts.
The first study (NCT04734145) seeks to enroll 110 adults with evidence of early-stage lung cancer, such as a suspicious, single nodule visible on a CT scan and an MSK radiology report of at least 50% certainty of suspected lung cancer or biopsy-proven early-stage lung cancer. Participants undergo an e-nose test during their presurgical visit before a cytohistological diagnosis is made. The trial is currently recruiting at various MSK locations in New Jersey and New York.
“More accurate and less invasive and costly methods for detecting lung cancer as early as possible will improve patient outcomes,” said Dr. Rocco. “We hope our evidence moves the field forward in establishing whether we may integrate e-nose technology into clinical practice in the future.”