MSK reaches more Spanish-speaking patients with game-changing genetic tests to improve their cancer treatment.
Ivan Marquez was sitting in the waiting room to see his prostate cancer doctor when his skills as a longtime coach kicked into gear. He noticed what he called a “newbie” sitting with a companion, the two of them whispering in Spanish.
“They were clearly petrified,” Ivan says. “So I went over to chat with them in Spanish to try to tranquillo them. I told them, ‘First of all, you’re in the best place on the planet to deal with it.’ ”
Before becoming a patient at Memorial Sloan Kettering Cancer Center (MSK), Ivan was a head coach for men’s college volleyball, so he knows how to talk people through stressful events. But more than that, Ivan is something of a cancer pro himself. He’s been living with stage 4 prostate cancer for more than 15 years.
He wasn’t always so calm under pressure, however. “When I first started coming in for treatment, I was scared of everything,” he says. “I couldn’t do a simple blood draw. I couldn’t do a simple biopsy. I caused the nurses many headaches by fainting a couple of times.”
Eventually, though, he learned to trust his treatment team, confident that they were giving him the best care possible. He calls his prostate cancer oncologist, Michael Morris, MD, his hero. “I’ve always had the attitude that whatever MSK advises me to do, they’re a good coach,” he adds. “I can coach basketball and volleyball. They can coach cancer.”
Now, in addition to giving impromptu pep talks to anxious patients, Ivan is also working with a team of researchers at the Robert and Kate Niehaus Center for Inherited Cancer Genomics at MSK. There, health psychologist Jada Hamilton, PhD, is focused on ensuring Spanish-speaking patients have equitable access to genetic counseling.
Achieving that goal is key to MSK’s mission to break down barriers to high-quality cancer care.
“We have to realize that the greatness of a place like MSK lies in our ability to treat people from every spectrum of life,” said Selwyn M. Vickers, MD, FACS, President and CEO of MSK, during his first Cancer Straight Talk from MSK podcast interview (episode 30, “Achieving Excellent Healthcare for All”). “There’s data to show that when you improve access for those who historically couldn’t get it, you improve the quality of care for everyone else as well. In fact, you make it better.”
Making Cancer Genetic Testing Easier
In this era of precision medicine, genetic testing is essential for people at high risk of developing cancer or already diagnosed with it. Genetic testing can:
- Directly influence a patient’s treatment options.
- Guide a prevention and surveillance plan for future cancer.
- Indicate whether family members are also at risk for cancer based on a genetic predisposition.
But many people have anxieties around genetic testing or simply lack accurate information. They might not take advantage of it because of scheduling conflicts, transportation limitations, or general mistrust of the medical establishment.
“We brought Ivan on as a patient representative to help us review our genetic testing information materials, to make them more accessible,” Dr. Hamilton says. “He has such a valuable perspective, coming from Puerto Rico and having experience being a patient at MSK himself — in addition to just being a lovely person with an amazing background. We made him a member of the Scientific Advisory Board for the studies we’re conducting.”
In particular, Ivan’s broad experience as a coach and his expertise in sports management (he has a graduate degree from the University of Southern California) lends itself perfectly to Dr. Hamilton’s research, which revolves around something called “mainstreaming” — to break down barriers to genetic testing.
The traditional process for genetic testing requires a few different meetings. First, patients have a pretest session with a professional genetic counselor to get basic information. Then, after the test, they need another session to understand the results and learn about treatment implications.
The mainstreaming model, piloted by Dr. Hamilton and her collaborators in the MSK Clinical Genetics Service, makes testing and the process of learning the results more convenient. Here’s how:
- The patient’s own cancer doctor gives them educational materials that cover the basics.
- They can give consent for testing on the spot to their doctor.
- Once the results are in, patients meet with MSK’s Clinical Genetics Service via a telemedicine session to discuss those results with a genetic counselor and a doctor.
Key to successfully broadening the reach of this approach is making sure that the educational materials are linguistically, culturally, and educationally appropriate. And that’s where Ivan’s expertise has been invaluable. “He’s able to put himself in the shoes of a patient and understand where they are coming from,” Dr. Hamilton says.
Ivan was able to advise Dr. Hamilton’s team on the best language to use, and even the best vehicle for delivering information. “We were trying to come up with something that can speak to all these people who are probably scared about finding out the results of the test,” Ivan says. “And that’s when we decided to create an animation that would explain the testing in friendly terms.”
Dr. Hamilton and her team of MSK co-investigators Kenneth Offit, MD; Mark Robson, MD; Jennifer Hay, PhD; and Zsofia Stadler, MD, are getting ready to open a clinical trial (research study) funded by a Cancer Moonshot grant from the National Cancer Institute to evaluate the mainstreaming approach in medically underserved patients, including those who speak Spanish or Haitian Creole, using the materials that Ivan helped develop.
Closing Gaps in Cancer Care
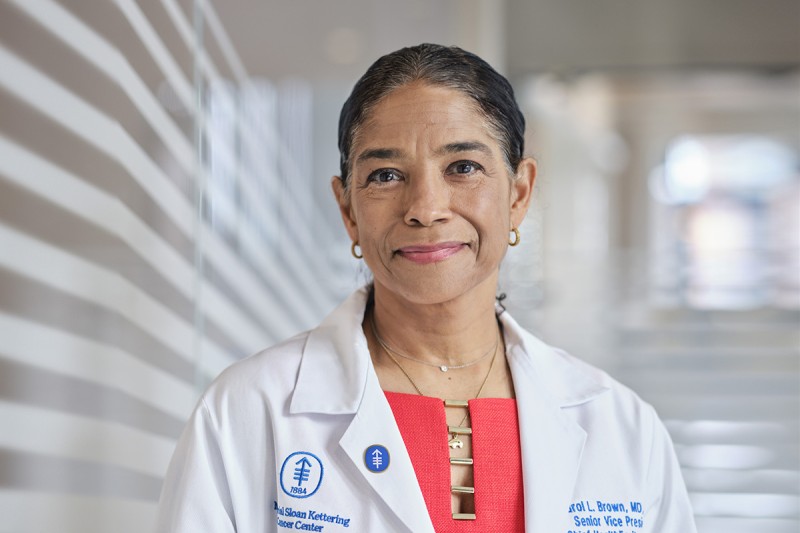
Dr. Hamilton’s work is just one of the ways that MSK is striving for better access for all. The Office of Health Equity has several initiatives to improve clinical care and research for people in underserved communities. In particular, the Cancer Health Equity Research Program (CHERP), led by Chief Health Equity Officer Carol Brown, MD, FACOG, FACS, is working to bring the benefits of advanced genetic testing to hospitals in historically underserved parts of the city, including the Queens Cancer Center and Kings County Hospital Center.
“Both of those hospital centers have very dedicated, outstanding oncologists,” Dr. Brown says. “But because they see the most underserved patients — who either have no insurance or are on Medicaid — they are limited in terms of the type of testing they can do and the sort of tools they can offer.”
That’s why, several years ago, as part of then Vice President Joe Biden’s Cancer Moonshot Initiative, Dr. Brown and her team launched a program called MSK-IMPACT To End Disparities (IMPACTED), in order to bring genetic testing to patients at these sites free of charge.
MSK-IMPACT® is MSK’s state-of-the-art genetic testing platform that looks for mutations (changes) in 500-plus genes that drive cancer. It helps doctors identify which new or experimental drugs a particular patient might benefit from, based on their unique tumor genetic profile. The test also is able to identify cancer mutations that a person may have inherited from their parents by sequencing normal cells from a patient, in addition to the cancer cells. In that way, it also identifies families who should consider more intensive screening based on having an inherited risk of developing cancer.
So far, the MSK-IMPACTED program has offered genetic testing to more than 600 patients at CHERP sites.
“We’re really proud of this effort to bring the latest, most advanced developments in treatment and prevention and genetic risk assessment to those patients who are the most vulnerable and who are the least likely to have access,” Dr. Brown says.
Diversity Leads to Discovery
Improving equity doesn’t end with improving access to genetic testing. There’s also the issue of follow-through. MSK gastrointestinal oncologist Zsofia Stadler, MD, who directs MSK’s Clinical Genetics Service, and her colleague, gynecological oncologist Ying Liu, MD, MPH, have found evidence that non-white people are less likely to follow up after genetic testing. They are also less likely to participate in “cascade testing,” which systematically identifies other family members who could be at risk from an inherited mutation.
“Genetic testing can help not just cancer patients but at-risk family members as well, to keep entire families healthy,” Dr. Stadler says. “Ultimately, testing cancer patients is a good start. But to make the most impact, we really need to be testing entire families.”
As to what explains this difference in follow-through, the researchers aren’t yet sure. “The next steps are to figure out what is driving this disparity and how we can fix it,” Dr. Liu says.
Beyond improving care for individuals and their families, there’s another major reason to pursue these projects: It’s good for science in general.
“We now are gaining more understanding that the diversity of our patients and our biospecimens is fundamental to the validity of our clinical trials,” Dr. Vickers shared with staff at an MSK town hall meeting. “Diversifying our patient population is not a peripheral exercise. It’s actually the core of what we do.”
Dr. Stadler agrees wholeheartedly. “We knew that we weren’t getting the full spectrum of inherited mutations in cancer patients because certain populations are underrepresented in our sample,” Dr. Stadler explains. “The MSK-IMPACTED program allows us to broaden our understanding of the diversity of mutations in all cancer patients by including more people.”
Ivan Passes the Ball Forward
Ivan is incredibly grateful for the care he has received at MSK, especially from Dr. Morris. “I know I wouldn’t be alive if it weren’t for him,” he says.
But it hasn’t been a one-way street when it comes to support. “I tell him, ‘I made you a star,’ ” Ivan says, beaming. He’s referring to the fact that he’s organized several fundraisers for Dr. Morris’ research and raised more than $25,000 through his many connections in the sports world and an extensive social media following. He counts both Walter the Howling Frenchie and Grumpy Cat (RIP) as followers of his Instagram.
Ever the coach, Ivan sees his advocacy work with Dr. Hamilton and MSK as just beginning. “I just want to do more,” he says.
Generous financial support for MSK-IMPACTED comes from Marie-Josée and Henry R. Kravis.
Dr. Brown holds the Nicholls-Biondi Chair for Health Equity at MSK.
Dr. Offit holds the Robert and Kate Niehaus Chair in Inherited Cancer Genomics.