Michael Morris, MD, says the new technology provides a major step forward in diagnosing and treating prostate cancer. “The benefits these advances will bring to men with this common disease cannot be overstated.”
Things were looking bleak for Michael Rosenblum in 2019. His prostate cancer had become resistant to chemotherapy and other treatments, and PET scans showed dark clusters of cancer cells in bones throughout his body. His prostate-specific antigen (PSA) level — a marker that should normally be in the single-digit range — had soared to more than 100. Most people in his condition would be out of options.
But his doctor, Memorial Sloan Kettering Cancer Center (MSK) medical oncologist Michael Morris, offered a lifeline: a new therapy that zeroes in on hidden prostate cancer cells to destroy them. The treatment, called 177Lu-PSMA-617, uses a molecule that selectively seeks out and attaches to a specific protein on the cancer cell surface called PSMA (prostate-specific membrane antigen). The technology delivers radiation that damages DNA and destroys the cancer cell.
Michael began treatment in July 2019 and finished in February 2020. After six doses of the therapy, the pictures spoke a thousand words: The dark clusters had vanished. His scans showed no visible signs of cancer. Michael celebrated his 50th wedding anniversary in 2021. The 76-year-old remains free of active disease, with a PSA that is undetectable.
“From how I feel today, you would never think I had cancer a few years ago,” he says.
“This type of precision medicine is a game changer for people whose prostate cancer has spread despite receiving multiple prior treatments,” Dr. Morris says.
An MSK Triumph
The PSMA-based technology could transform care for prostate cancer, the second leading cause of cancer death in American males. The PSMA molecule was first identified at MSK in the early 1990s. Since then, MSK has continued to play a critical role in developing and testing this technology to track and treat spreading prostate cancer cells, which would otherwise be hidden.
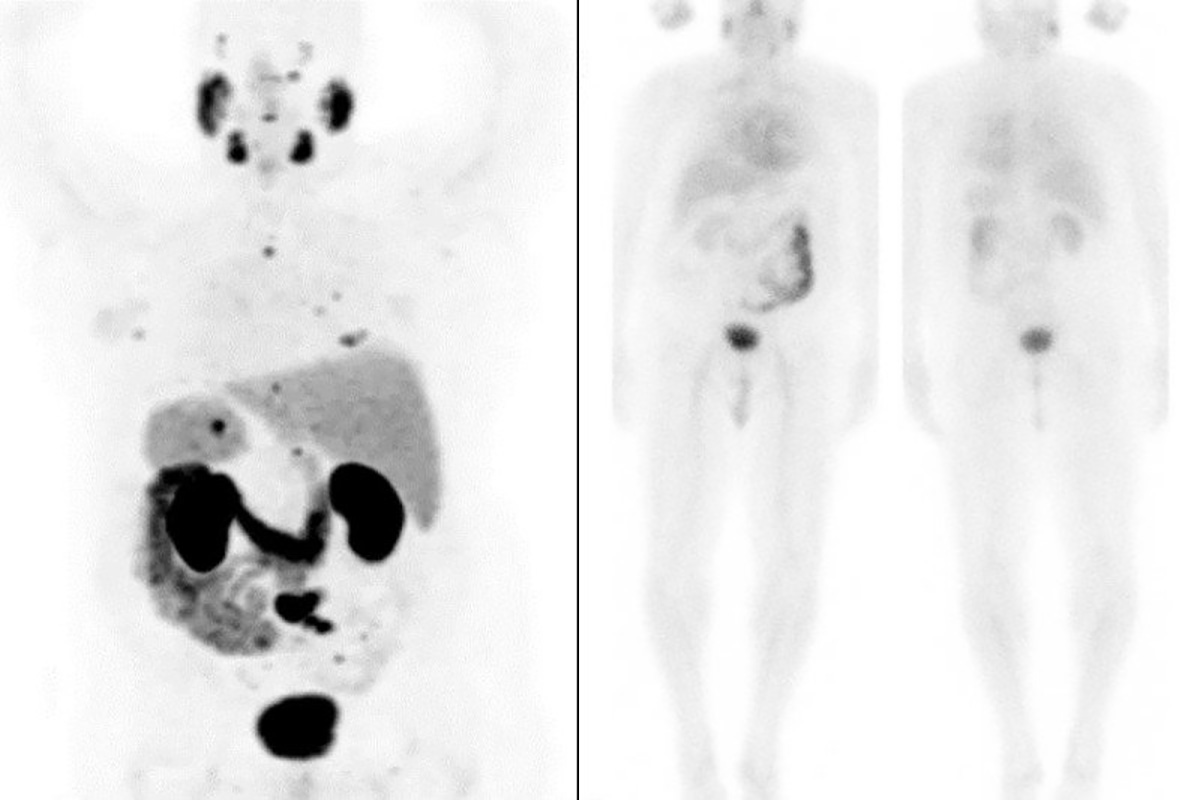
(Left) PSMA PET scans of Michael Rosenblum before treatment show prostate cancer metastases (small dark spots) throughout his body. (Right) After treatment, metastatic cancer is no longer visible
The initial breakthrough involved using a radioactive substance, or tracer, to find metastatic prostate cancer cells. Dr. Morris played a leading role in clinical trials testing a particular tracer that gained FDA approval in 2021.
“This is the biggest diagnostic advance for prostate cancer since the 1980s, when the PSA test was introduced,” he says. “Imaging has been the Achilles’ heel of prostate cancer, forcing many treatment choices to be based on estimation and probabilities. Now, we can be much more confident that we are correctly identifying the location of the disease to make an accurate treatment plan.”
Creating the technology that pinpoints these elusive cells was a total team effort: The MSK Molecular Imaging and Therapy Service, led by Heiko Schöder, was key in testing the tracer, as were MSK radiologist Hebert Alberto Vargas and interventional radiologist Jeremy Durack.
“This advance is the result of years of work by the community of physicians promoting the use of PSMA agents,” Dr. Schöder says. “It’s gratifying to see a collaborative effort result in a breakthrough that has the potential to make a difference for so many patients with advanced prostate cancer.”
The Promise of Theranostics

Lisa Bodei, MD, PhD, Director of Targeted Radionuclide Therapy
The technology has exciting potential for other cancers, too. It represents the latest bold advance in the emerging field of theranostics, which uses radioactive substances to visualize cancer cells and destroy them without harming normal cells.
“We have a theranostic motto, which is ‘We see what we treat, and we treat what we see,’” says nuclear medicine physician Lisa Bodei, Director of Targeted Radionuclide Therapy at MSK. She specializes in using radioactive materials to diagnose and treat cancer and played a key role in the MSK clinical trial for prostate cancer.
Here’s how it works: First, patients are scanned to make sure there is enough PSMA present in the cells to make them likely to respond to the treatment. Then, patients receive the radioactive drug by injection over four to six sessions, spaced six weeks apart.
“I had no side effects, either on the day of the procedures or afterward,” Michael says. “My PSA went right down, and my blood tests have been really good.”

Michael Rosenblum
The trial also showed that adding the drug to standard treatment slowed progression of prostate cancer. Dr. Morris presented the results in June 2021 at the annual meeting of the American Society of Clinical Oncology. They also were reported in The New England Journal of Medicine. The FDA approved 177Lu-PSMA-617 for therapeutic use in March 2022.
“This enables even more people who had essentially been given death sentences to survive and live well,” Dr. Morris says. As a next step, he and colleagues are looking into using the PSMA-directed therapy earlier — rather than only after the prostate cancer has spread.
For Dr. Morris, the recent inroads against this stubborn disease are especially gratifying. “I have been involved in the PSMA research since the end of my fellowship at MSK in the late 1990s,” he says. “It’s amazing to see it all come to fruition. The benefits these advances will bring to men with this common disease cannot be overstated.”
What Lies Ahead: Leading the Way With Alpha Therapies

Jason Lewis, PhD, is a radiochemist who develops radiopharmaceuticals to treat cancer
The theranostics advances will continue with even more powerful forms of radioactive therapy. The MSK laboratory of radiochemist Jason Lewis (Emily Tow Jackson Chair in Oncology) and other researchers are investigating the use of alpha particles, which are hundreds of times more potent than the photons used in conventional radiation. Not only do alpha particles cause more damage when they slam into cancer cells but their path of destruction is also more tightly focused, sparing normal cells.
MSK is building one of the nation’s first dedicated alpha particle labs at a U.S. academic institution that meet the standards set by the U.S. Food and Drug Administration (FDA) for clinical application.
“These radiopharmaceuticals that we are creating translate very well from bench to bedside,” says Dr. Lewis, Chief of the Radiochemistry and Imaging Sciences Service and Director of the Radiochemistry and Molecular Imaging Probe Core Facility. “When you see these striking responses to treatment, it brings real hope for the future and our patients.”
Michael Rosenblum couldn’t agree more.
The Magnier family and the Scannell family have provided vital support for prostate cancer research at MSK.
Advances in radiotheranostics are supported by The Tow Foundation, long-time contributors to MSK’s mission.