
Since 1945, the Sloan Kettering Institute has championed a scientific approach to solving the cancer problem.
When General Motors executive Alfred Sloan, Jr., and engineer Charles Kettering announced the formation of the Sloan Kettering Institute (SKI) in 1945, they hoped to translate the organizational skills they honed in the automobile industry to the fight against cancer. “I am inclined to feel we can apply some of our time-tried techniques to this age-old problem,” Mr. Kettering said.
In essence, that meant providing scientists with the time, financial support, and technological resources to do what they do best: conduct research.
As an institute devoted to research, SKI’s mission has always been to supply the raw material of discovery out of which new approaches to cancer treatment, diagnosis, and prevention emerge. The first chemotherapy drugs, the first immune-based treatments for cancer, and a variety of targeted therapies all had their origins at SKI.
Timeline Transcript
—Timeline of Progress
Click right to view major scientific milestones of the Sloan Kettering Institute.
—The Sloan Kettering Institute is established
On August 8, 1945 — two days after the atomic bombing of Hiroshima — General Motors executive Alfred P. Sloan, Jr., and engineer Charles F. Kettering announce the creation of the Sloan-Kettering Institute for Cancer Research. The two founders seek to apply lessons gleaned from the automobile industry to cancer research.
—The Sloan Kettering Institute opens its doors
As conceived by its founders, the Sloan Kettering Institute would be devoted solely to scientific research and would serve as both the physical and intellectual center of MSK. "The Sloan Kettering Institute building will stand squarely in the middle of Memorial Cancer Center," Reginald Coombe, Memorial's president, said at the time.
—First chemotherapy drugs developed
Between 1946 and 1959, SKI investigators test thousands of natural and synthetic chemicals that they hope might selectively kill cancer cells, while leaving normal cells unharmed. This large-scale screening program brings to oncology some of the first effective chemotherapy drugs, including 6-mercaptopurine and the nitrogen mustards.
—Viral cause of leukemia discovered
Virologist Charlotte Friend identifies a virus that causes leukemia in mice. Her work lends strong support to the controversial idea that viruses can cause cancer. The virus she discovered is now known as the Friend leukemia virus.
—BCG found to boost immune response to cancer
Immunologist Lloyd J. Old discovers that certain bacterial products can boost an animal’s innate immunity to cancer. Mice injected with a weakened version of a bacterium called Bacillus Calmette-Guerin (BCG) are resistant to the growth of implanted tumors. This discovery marks the beginning of modern tumor immunology.
—Horsfall becomes SKI Director
Pioneering virologist Frank Horsfall becomes director of SKI. During his tenure, he encourages the study of virology and immunology.
—T cell subtypes identified
Geneticist Edward (Ted) Boyse and immunologist Lloyd Old use antibodies to identify surface markers on different functional subsets of T cells. This paves the way for the cluster of differentiation, or CD, system for identifying T cells, such as CD4 and CD8.
—Good becomes SKI Director
In 1968, physician-scientist Robert Good performed the first successful bone marrow transplant from a sibling, permanently curing a boy born with severe combined immunodeficiency. At SKI, he continues to research and develop the science of bone marrow transplantation.
—Cancer-killing immune molecule identified
Lloyd Old, Elizabeth Carswell, and colleagues identify tumor necrosis factor (TNF), a powerful immune system molecule that causes tumors to hemorrhage and die. This work provides a clear link between the immune system and cancer.
—Role of interferons in cancer explored
Virologist and geneticist Mathilde Krim was influential in promoting the study of interferons and cancer. She was a member of SKI from 1962 to 1985. In 1983, she cofounded the AIDS Medical Foundation (later the American Foundation for AIDS Research, or amfAR) to raise money and support AIDS research.
—Flu virus replication unlocked
Molecular biologist Robert Krug, who was a member of SKI from 1967 to 1989, discovers the process of "cap-snatching," by which the influenza virus tricks a host cell into making new proteins from its messenger RNA. A drug targeting this process (Xofluza) was approved in 2018 as a treatment for the flu.
—Marks named president of MSK
Basic science at SKI grows dramatically under the leadership of Paul Marks, who became president of MSK in 1980. In his own research, Dr. Marks made important contributions to the early understanding of epigenetic changes in cells. The FDA-approved drug vorinostat (Zolinza) is based on his work.
—MYC oncogene discovered
Molecular biologist William Hayward, working with scientists at The Rockefeller University, discovers that mutations in a gene called MYC can cause cancer, pinpointing it as an oncogene.
—Rifkind becomes SKI Director
Richard Rifkind, who had been a colleague of Paul Marks when they were at Columbia University, becomes the fourth SKI director. He serves from 1983 to 1999.
—Expert in RNA polymerase joins SKI
Biochemist Jerard Hurwitz, who co-discovered RNA polymerase in 1960, comes to SKI in 1984 as part of an effort to grow the molecular biology program.
—Human G-CSF purified
Physician-scientists Malcolm Moore and Karl Welte isolate a protein from human cells that stimulates new blood cell growth. Called G-CSF, this protein forms the basis of filgrastim (Neupogen), one of the most important cancer drugs ever developed.
—Gene for insulin receptor cloned
Biochemist Ora Rosen, working in collaboration with researchers at Genentech, clones the gene for the insulin receptor, the molecule to which the insulin hormone binds and through which it signals to the cell.
—Process of DNA replication described
Molecular biologist Ken Marians, who arrived at SKI in 1984, makes numerous contributions to the understanding of how prokaryotes replicate their DNA. His research shows that the process is intrinsically tolerant of DNA damage, and that there are various ways to bypass it.
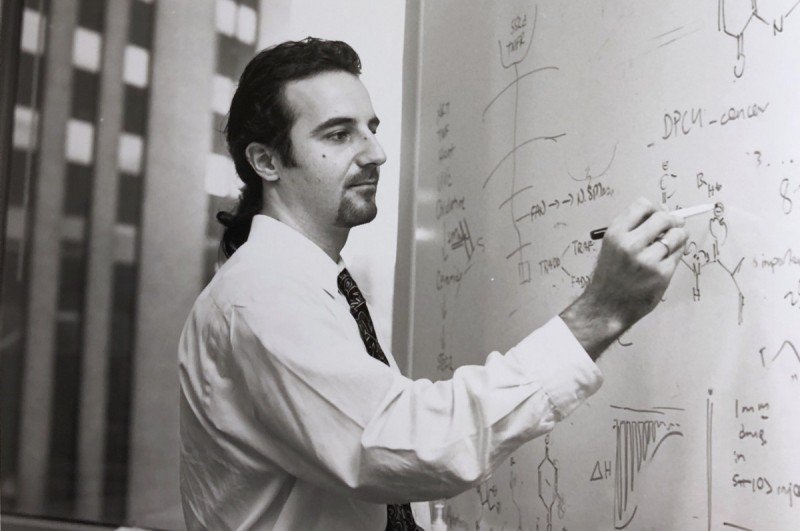
—EGFR-targeted therapy pioneered
Physician-scientist John Mendelsohn, who co-led the SKI Molecular Pharmacology Program from 1985 to 1990, developed the concept of using antibodies to block the epidermal growth factor receptor (EGFR) as a way to treat cancer. At MSK, he conducts important laboratory research and, with MSK colleagues, spearheads pivotal clinical trials that spur the development of the EGFR-blocking drug cetuximab (Erbitux). This work blazes a path for other growth factor receptor-targeting drugs such as trastuzumab (Herceptin).
—Protein transport deciphered
Biochemist James Rothman teases apart the mechanism that cells use to package and transport proteins. For this work, he shared the 2013 Nobel Prize in Physiology or Medicine. Dr. Rothman was a member of SKI from 1991 to 2003 and founding chair of the Cellular Biochemistry and Biophysics Program.
—TGF-beta pathway delineated
Cell biologist Joan Massagué delineates the TGF-beta signal transduction pathway from membrane receptors to nuclear targets, establishing the central concept for how this family of pleiotropic signals controls stem cell division, immunity, and metastasis. Dr. Massagué arrived at SKI in 1989, becoming chair of the Cell Biology Program.
—Structure of p53 determined
Nicknamed the "guardian of the genome," the p53 gene is mutated in more than half of all cancers. Using X-ray crystallography, structural biologist Nikola Pavletich determines the structure of the p53 protein, showing how it binds to DNA, a major milestone in cancer research.
—Epothilones synthesized
Organic chemist Samuel Danishefsky synthesizes a type of cancer drug called an epothilone, which exhibits a manner of cell killing similar to that of the chemotherapy drug Taxol.
—BRCA2 mutation identified
Cancer geneticist Kenneth Offit, who has a joint appointment in the Cancer Biology and Genetics Program at SKI, discovers the most common mutation of BRCA2. This inherited mutation is associated with a much higher risk of breast and ovarian cancers in women.
—Signal for limb development discovered
Developmental biologist Lee Niswander shows that bone morphogenetic protein (BMP) controls the programmed cell death that occurs between the digits of the developing chick limb. Blocking BMP signaling results in chicks with webbed feet, similar to what is seen in ducks.
—Expert in gene regulation comes to SKI
Molecular biologist Mark Ptashne, who won the Albert Lasker Award for Basic Medical Research in 1997, joins SKI the same year. Through his work on the lambda repressor, conducted at Harvard, Dr. Ptashne showed how gene transcription — turning genes on and off — could be regulated by a simple "molecular switch" composed of proteins binding specifically to DNA.
—Delineating the SPO11 mechanism of meiotic recombination
Molecular biologist Scott Keeney demonstrates how Spo11, a member of a widely conserved protein family, catalyzes DNA double-strand breaks (DSBs) that are specific to meiosis. This work is the first identification of a biochemical function for any of the gene products involved in DSB formation.
—Role of BRCA1 gene established
Molecular biologist Maria Jasin uses a mouse model to show that the BRCA1 protein is necessary for the repair of double-strand breaks in DNA by homologous recombination. Inherited mutations in the BRCA1 and BRCA2 genes are responsible for a large share of familial cancers.
—Varmus becomes MSK President
As president of MSK from 2000 to 2010, physician-scientist Harold Varmus greatly expands the institution's research efforts. Dr. Varmus, together with J. Michael Bishop, discovered that the proto-oncogene src is a normal part of cellular DNA. For this work, they were awarded the Nobel Prize for Physiology or Medicine in 1989.
—Alpha particles harnessed as therapy
David Scheinberg and colleagues publish the first practical methods for selectively targeting highly potent alpha particles, derived from Department of Energy programs, to various cancers. Clinical trials in people with leukemia soon follow.
—Chimeric antigen receptor (CAR) T cells developed
Michel Sadelain, Renier Brentjens, and Isabelle Rivière develop genetically engineered T cells with a chimeric antigen receptor (CAR), now a powerful way to fight leukemia and other blood cancers. CARs are hybrid proteins made up of different immune molecules joined together.
—Kelly becomes Director of SKI
Molecular biologist Thomas Kelly joins SKI as director after a 30-year career at the Johns Hopkins University School of Medicine. Dr. Kelly helps to strengthen the basic science programs at SKI by recruiting many new investigators to the institution.
—Center for Experimental Therapeutics established
Founded and directed by molecular pharmacologist David A. Scheinberg, this center is the first and largest of several collaborative research centers to be established at MSK. Its purpose is to encourage drug development and speed the translation of discoveries from the laboratory to the bedside.
—Anderson becomes Chair of Developmental Biology
Kathryn Anderson, a prominent developmental biologist who had been at SKI since 1996, becomes the first female chair of an SKI program, Developmental Biology, in 2003.
—Allison becomes Chair of Immunology
Immunologist James Allison joins SKI to help steer the clinical development of a new drug that blocks a molecule on immune cells called CTLA-4. Dr. Allison was the first to show, in 1996, that blocking CTLA-4 could cure cancer in mice. The new drug, called ipilimumab, opens up a whole new approach to cancer treatment geared toward “releasing the brakes” on the immune system. Dr. Allison, along with Tasuku Honjo, won the 2018 Nobel Prize in Medicine or Physiology for this work.
—Adaptive resistance to signaling inhibition defined
Molecular pharmacologist Neal Rosen shows how inhibiting different parts of the RAS-RAF-MEK-ERK and PI3K-AKT-mTOR pathways with targeted drugs leads to feedback allowing cancers to adapt to these drugs.
—First HDAC inhibitor approved
Former MSK President and physician-scientist Paul Marks conducts laboratory work leading to the development of the first HDAC inhibitor, called SAHA or vorinostat. This drug works by targeting an enzyme called histone deacetylease, altering the way DNA is wrapped around proteins called histones. Marketed by Merck as Zolinza, the drug was approved in 2006 for the treatment of advanced refractory cutaneous T cell lymphoma.
—Hedgehog signaling found to depend on primary cilium
Developmental biologist Kathryn Anderson shows that an important signaling protein in mammals, Hedgehog, depends on a cell structure called the primary cilium for its action.
—Structure of histone reader determined
Structural biologist Dinshaw Patel, working with David Allis at The Rockefeller University, determines the structure of a protein that binds to and reads the instructions imprinted on histones, DNA’s packaging proteins. The research reveals new mechanisms by which some diseases, including certain types of leukemia, may arise.
—Rudensky elucidates regulatory T cells
Immunologist Alexander Rudensky, who joined SKI in 2009, is a world expert on the biology and function of regulatory T cells (Tregs), an important subset of immune cells that help keep the immune system in check. Understanding Tregs has implications for treating cancer as well as autoimmune diseases.
—Thompson becomes president of MSK
MSK President and Member of the SKI Cancer Biology and Genetics Program Craig Thompson is recognized for having rekindled interest in cancer metabolism as a means to understand and treat the disease.
—Ipilimumab approved for treatment of melanoma
Ipilimumab (Yervoy®), the first immune checkpoint inhibitor, is approved by the FDA for the treatment of advanced melanoma, based on clinical trials led by Jedd Wolchok, a joint member of the SKI Immunology Program. Patients at MSK began receiving ipilimumab in 2004, under the care of Dr. Wolchok. These patients are some of the earliest patients in the world to receive this drug, and a number of them are still alive today.
—Lowe joins SKI
Biologist Scott Lowe joins MSK in 2011. While a graduate student at the Massachusetts Institute of Technology, together with his advisor, Tyler Jacks, Dr. Lowe showed that p53 is required for the cell-killing action of certain chemotherapy drugs. DNA damage triggers p53 to induce the cell to commit suicide.
—Stem cell technique creates dopamine-producing neurons
Stem cell biologist Lorenz Studer shows that embryonic stem cells can be induced to create dopamine-producing neurons that can grow and survive long term after being transplanted into the living brains of animal models. The discovery holds promise for treating the degenerative neurological disorder Parkinson’s disease.
—Massagué becomes SKI Director
Joan Massagué, who joined SKI in 1989, becomes its director in 2014. Dr. Massagué is internationally known for his work on the TGF-beta family of growth factors and his contributions to the growing understanding of the biology of metastasis. He launches new SKI programs and collaborative research centers and increases interactions between experimental and clinical researchers at MSK.
—Toll receptor code found to shape fly embryo development
SKI development biologist and Howard Hughes Medical Institute Investigator Jennifer Zallen discovers that receptor proteins of the Toll family direct the oriented cell rearrangements required for the elongation of the head-to-tail axis during Drosophila development.
—How cancer cells spread to the brain and thrive
SKI Director Joan Massagué identifies genes and proteins that control the survival of metastatic breast and lung cancer cells in the brain. These survival factors might one day be targeted with drugs to further diminish people’s risk of metastasis.
—Restoring a gene's activity found to turn cancer cells normal
Scott Lowe, an expert in genetic models of cancer, finds that restoring the activity of a gene called APC, which is often mutated in colorectal cancer, turns the cells to normal.
—Pe'er joins SKI
Dana Pe’er becomes Chair of the Computational and Systems Biology Program and launches a research program to decipher the identity and activity of thousands of individual cells, both cancerous and noncancerous, in human tumor samples.
—SKI acquires cryo-electron microscope
SKI purchases an FEI Titan Krios cryo-electron microscope with a Gatan K2 Summit detector. This powerful device promises to greatly enhance scientists’ ability to understand the structure and function of biological molecules, including those that malfunction in cancer.
—Complete structure of mTORC1 determined
Using cryo-electron microscopy, and building on their earlier X-ray crystallography work, SKI scientists including Nikola Pavletich and Haijuan Yang solve the complete structure of mTORC1, a key regulator of cellular growth.
—First CAR T therapies approved
The FDA approves two chimeric antigen receptor (CAR) T therapies for blood cancers. This approach was pioneered by SKI scientists Michel Sadelain, Isabelle Rivière, and Renier Brentjens.
—IDH inhibitor approved
The US Food and Drug Administration approves the drug enasidenib (Idhifa) for the treatment of IDH-mutant acute myeloid leukemia that has stopped responding to other therapies. Cancer biologist and immunologist Craig Thompson did much of the preclinical work deciphering the relationship between the IDH mutations and cancer, including work done while he was at the University of Pennsylvania.
—Basis for T cell exhaustion clarified
Immunologist Andrea Schietinger reports that T cells become dysfunctional through successive waves. When T cells enter tumors, they quickly lose their ability to kill cancer cells, but their fate is plastic — there is an early window in which they can still be reactivated. But with time, the T cells become exhausted and settle into a fixed state in which they cannot be reprogrammed. This informs effective use of checkpoint inhibitors.
—New organelle called TIGER domain discovered
SKI scientists Christine Mayr and Weirui Ma discover a new cell part, or organelle, called the TIGER domain, which is where mRNA finds the appropriate environment in which to grow up. The TIGER domain acts as a sorting mechanism that shapes how proteins will function.
—Discovering keys to inflammatory immune response
SKI chemical biologist Daniel Bachovchin and colleagues make important discoveries about how small molecule inhibitors activate the NLRP1B inflammasome, triggering a fiery form of cell suicide called pyroptosis. The work has major implications in understanding the innate immune response and provides new avenues to develop therapeutics for acute myeloid leukemia.
—Development of senolytic CAR T cells
SKI cancer biologist Scott Lowe, physician-scientist Michel Sadelain, and colleagues develop breakthrough chimeric antigen receptor (CAR) T cells that can selectively target and eliminate senescent cells in mouse disease models, reversing disease and extending survival. Developing senolytic agents to selectively target senescent cells has potential relevance for diseases beyond cancer, including fibrosis, atherosclerosis, and osteoarthritis.
—A novel treatment strategy for leptomeningeal metastasis
SKI computational biologist Dana Pe’er and MSK neuro-oncologist Adrienne Boire discover that leptomeningeal metastasis cells reprogram themselves to outcompete surrounding cells for iron in order to survive. The team identifies iron chelation as a novel therapeutic approach for the lethal disease.
—How the gut microbiome affects response to cancer treatments
SKI systems biologist Joao Xavier, along with Marcel van den Brink, demonstrate how the gut microbiome can be reconstituted in precise ways to restore a healthy system after a bone marrow transplant. They also show that the concentration of different types of immune cells in the blood changes in relation to the presence of different bacterial strains in the gut, explaining how they impact both transplant-related mortality and responses to cancer immunotherapy.
—Hedgehog under the microscope
A team led by SKI structural biologist Stephen Long uses cryogenic electron microscopy (cryo-EM) to reveal the inner workings of the assembly machinery for Hedgehog proteins. The technology enables them to probe the shapes of the proteins more completely than ever before.
—Novel mechanisms of metabolism
A team led by SKI immunologist Ming Li discovers a new reason why fast-dividing cells, like cancer and immune cells, rely on Warburg metabolism. They identify a link between Warburg metabolism and the activity of the cell enzyme called PI3 kinase. This may help explain why cancer cells have a great appetite for sugar.
—Retooling CAR T cells to serve as 'micropharmacies'
SKI chemical biologist Derek Tan, in collaboration with SKI molecular pharmacologist David Scheinberg, develops a novel class of CAR T cells engineered to biosynthesize small-molecule drugs with synergistic anti-tumor activity locally at tumor sites. The platform, called SEAKER, could offer a way to overcome key limitations of current CAR T cell therapies.
—Redefining the Krebs cycle
Cell biologist Lydia Finley discovers an alternate version of the Krebs cycle, which allows cells to use carbons from sugar to build molecules such as lipids. The finding has broad implications for understanding how cells adapt their metabolisms to meet changing needs.
—New rules for the 'guardian of the genome'
A study led by SKI cancer biologist Scott Lowe finds that loss of p53 is followed by an orderly progression of predictable genetic changes — not genetic chaos, as previously believed. Discovering that there are “rules” to the genetic evolution of tumors suggests a different way of thinking about treating them.
—Solving the structure of the RNA exosome
Structural biologist Christopher Lima uses cryo-electron microscopy and other methods to illuminate the RNA exosome and its components. RNA degradation pathways are highly regulated and control everything from embryonic development to the progression of the cell cycle. His team was able to decipher the structure of a protein assembly called Nuclear Exosome Targeting (NEXT) Complex, a key part of the degradation machinery.
—How prostate cancer cells activate lineage plasticity
Research done in laboratory models and led by physician-scientist Charles Sawyers and SKI computational biologist Dana Pe’er finds that prostate cancer cells undergo lineage plasticity, converting to a new cell type, by activating inflammatory signaling pathways JAK/STAT and FGFR. Blocking the pathways resensitizes the cancer cells to therapy — potentially opening the door to new clinical approaches.
- The first chemotherapy drugs, including the nitrogen mustards and 6-MP
- Neupogen (filgrastim), a drug that helps blood cell counts recover after chemotherapy
- Vorinostat (Zolinza), the first HDAC inhibitor
- Ipilimumab (Yervoy), the first immune checkpoint inhibitor
- Chimeric antigen receptor (CAR) T cells, sometimes called “living drugs”
1945–1959: Birth of Chemotherapy
Nothing better illustrates the early aspirations of the institute than the search for effective chemotherapeutic drugs. This massive program involved screening more than 50,000 natural and human-made chemicals for their effectiveness as anticancer drugs. It would lead to the development of some of the first approved chemotherapy drugs, and also served as a model for a similar program at the National Cancer Institute.
SKI’s first director, a pathologist named Cornelius Rhoads, had served as chief medical officer of the Army’s Chemical Warfare Service during World War II. From this post, he learned about the effects of chemical weapons, such as mustard gas, on human physiology. Research in this area eventually led to the development of the class of chemotherapy drugs called the nitrogen mustards. Dr. Rhoads’s ties to the military and charges of unethical human experimentation would later sully his reputation as a pioneer of chemotherapy.*
SKI also supported the work of chemists Gertrude Elion and George Hitchens at Burroughs Wellcome, which produced the chemotherapy drug 6-mercaptopurine (6-MP). MSK oncologists Joseph Burchenal and David Karnofksy led the testing of this new compound in people with leukemia. Based on this work, the US Food and Drug Administration approved 6-MP in 1953.
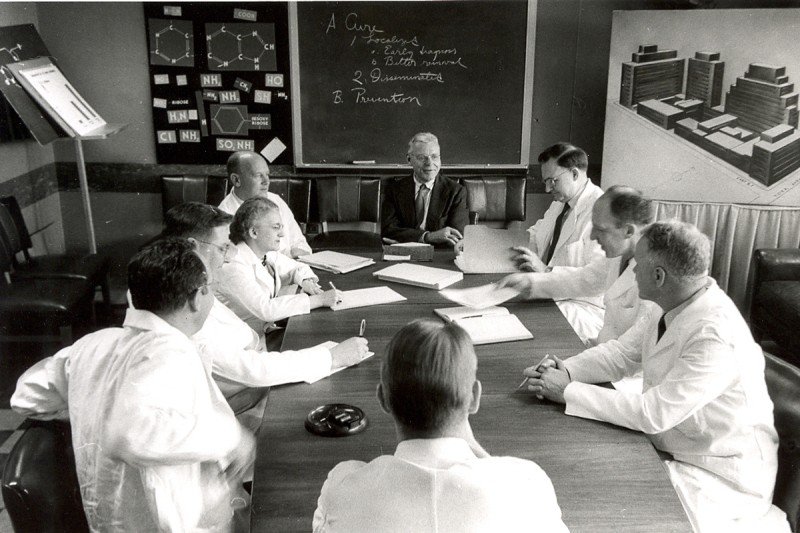
SKI scientists were pioneers of chemotherapy for cancer. Pictured here (from left to right) are Fred Philips, John Biesele, Christine Reilly, Joseph Burchenal, Cornelius Rhoads, C. Chester Stock, David Karnofsky, and George Woolley.
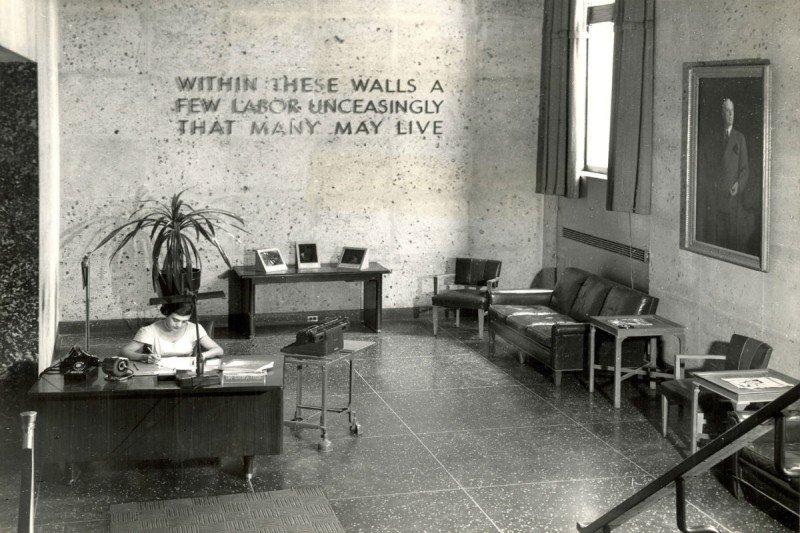
A view of the SKI lobby in 1949. The inscription reads: Within These Walls A Few Labor Unceasingly That Many May Live.

SKI pathology lab, 1950
In 1958, a young medical doctor joined the experimental chemotherapy division at SKI. His interests were slightly different from those of his fellow chemotherapists. What captured Lloyd Old’s imagination was the idea that the immune system could fight cancer.
In 1959, Dr. Old, along with his colleagues Baruj Benacerraf and Donald Clarke, showed that mice injected with a germ called BCG could fight off transplanted tumors and resist new tumors forming. This was a seminal moment in immunotherapy. Dr. Old is considered the father of modern tumor immunology.
1960–1979: Viruses, Cancer, and Immunity
Dr. Rhoads, SKI’s first director, died suddenly in 1959. Replacing him, in 1960, was Frank Horsfall, a pioneering virologist who had studied the influenza virus at the Rockefeller Institute, next door to Memorial Hospital. As director, Dr. Horsfall encouraged the study of virology and immunology at SKI.
He supported the work of several scientists who were studying the relationship between viruses and cancer, for example, including Alice Moore, Charlotte Friend, and Chester Southam. These researchers identified cancer-causing viruses and, conversely, also showed that infection with some viruses causes cancers to regress. These developments were a forerunner of today’s oncolytic virus therapies.
Having established in 1959 that the immune system could fight cancer, SKI immunologist Lloyd Old next went in search of distinguishing cancer markers, or antigens, and the cell types involved in immune recognition. In the early 1960s, with SKI geneticist Edward (Ted) Boyse, he identified cancer antigens associated with chemically induced and virally caused cancers. Later, the same team discovered that immune cell types could be distinguished by specific cell-surface markers, which led to the identification of CD8+ “killer” T cells and CD4+ “helper” T cells.
Lloyd Old (left) with Helen Coley Nauts. Dr. Old is considered the father of modern tumor immunology.
Robert Good was director of SKI from 1973 to 1980.
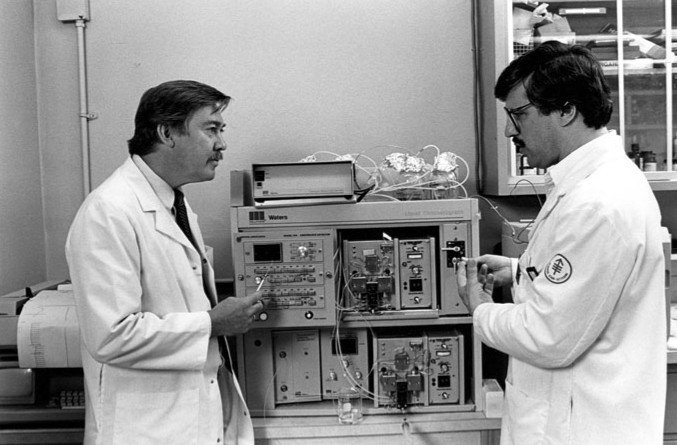
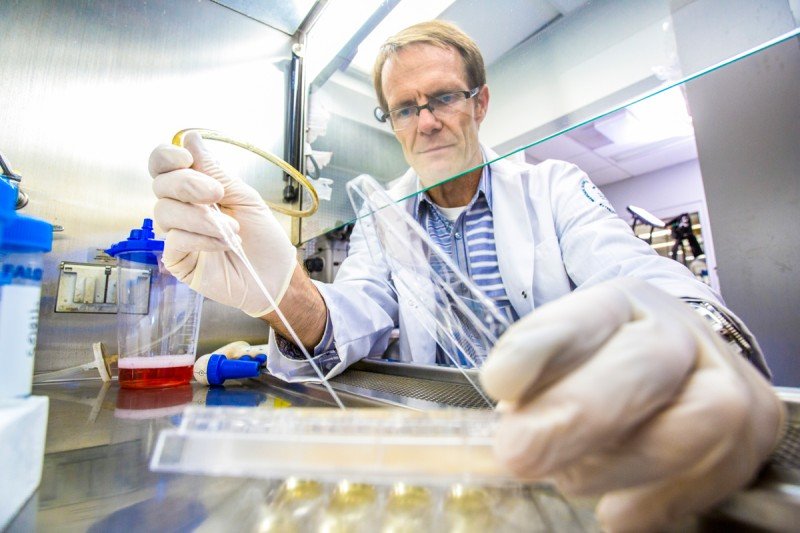
Malcolm Moore (left) and Karl Welte conducted work leading to the development of Neupogen (filgrastim).
The immunological focus of the institute continued under its third director, Robert Good, who served from 1973 to 1980. Dr. Good was a pioneer of bone marrow transplantation, having achieved the first successful cure of a boy with an immune disorder called SCID.
Hematologist and cell biologist Malcolm Moore came to SKI in 1974. Work that he conducted on factors that stimulate blood growth would lead to the development of the drug Neupogen (filgrastim). This widely used medicine helps blood cell counts recover after chemotherapy, reducing the risk of infection and hospitalization. It is one of the most important cancer drugs ever developed.
1980–1999: Getting Molecular
By the end of the 1970s, the field of molecular biology was exploding, offering new ways to understand and manipulate the DNA within cells. SKI would need to make some changes to take advantage of the new perspective.
The person who did the most to bolster SKI’s expertise in molecular biology was Paul Marks, a physician-scientist who served as MSK’s president from 1980 to 1999. It was Dr. Marks’s belief that this area held great promise for understanding and treating cancer.
Dr. Marks’s views on cancer research were shaped in part by his own introduction to molecular biology, through time he spent in the Pasteur Institute lab of the Nobel Laureate Jacques Monod in the 1960s. He wanted to bring that perspective to MSK.
“Most of the answers to cancer lie down on the level of the genes, in our understanding of how cells differentiate and divide,” Dr. Marks once said. He appointed physician-scientist Richard Rifkind director of SKI in 1983 to help him grow the institute. Dr. Rifkind was a colleague from Columbia, where both he and Dr. Marks were faculty before coming to MSK.
Among the talented scientists that they recruited to SKI in the 1980s were Jerard Hurwitz and Ora Rosen, who founded the Molecular Biology Program. Dr. Hurwitz had co-discovered the enzyme RNA polymerase in 1960. Dr. Rosen was a world expert in the biology of hormones. In 1985, Dr. Rosen was part of a team, including members of the newly founded company Genentech, that cloned the gene for the insulin receptor.
Cancer biologist Joan Massagué arrived at SKI in 1989 as the new chair of the Cell Biology Program. After joining SKI, Dr. Massagué elucidated the transforming growth factor beta (TGF-beta) signaling pathway. This pathway controls several aspects of cell behavior and is often derailed in cancer.
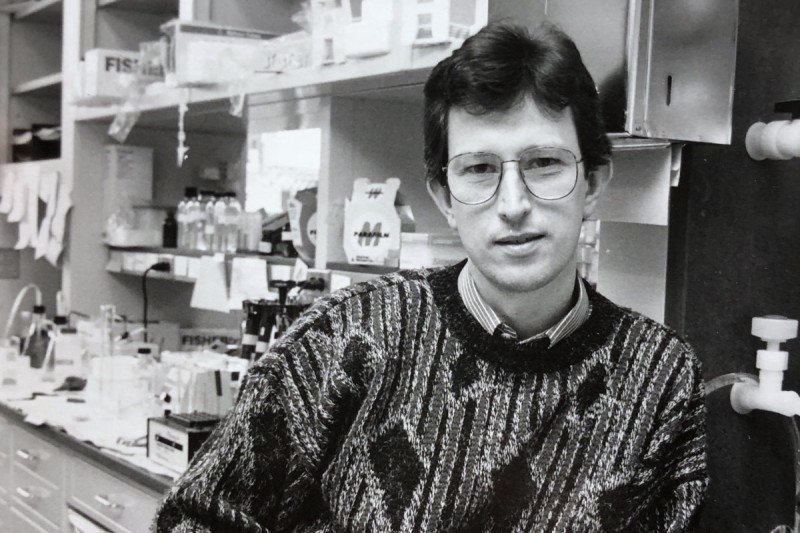
Structural biologist Nikola Pavletich solved the three-dimensional structure of p53.
Cell biologist Joan Massagué elucidated the TGF-beta pathway.

Biochemist Ora Rosen (right) deciphered how insulin signaling works.
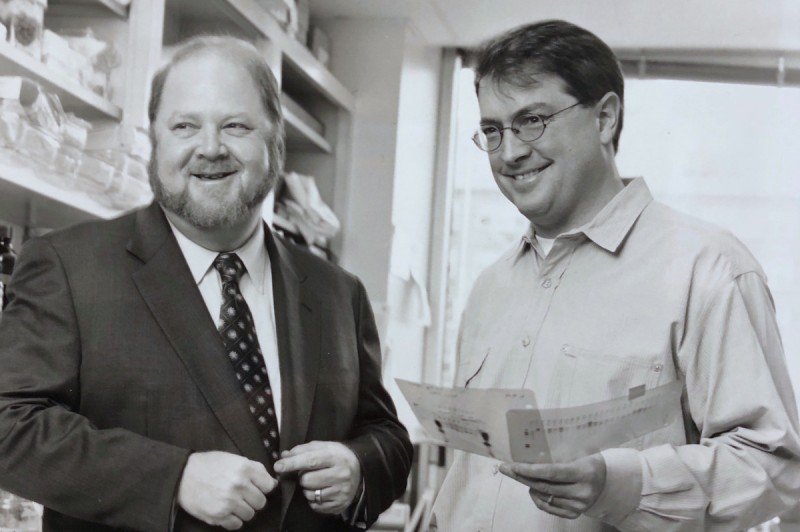
Cell biologist James Rothman (left) won a Nobel Prize for his work on protein trafficking. Dr. Rothman is seen here with Carl Blobel.
The 1990s witnessed substantial growth in biochemistry and biophysics. James Rothman arrived in 1991, becoming founding chair of the Cellular Biochemistry and Biophysics Program. A giant in the field, Dr. Rothman would go on to receive a Nobel Prize, in 2013, for his work on protein trafficking done at SKI.
Structural biology also gained momentum at this time. One of the first recruits, Dinshaw Patel, did some of the earliest work linking chemical carcinogenesis to DNA binding. Another, Nikola Pavletich, deciphered the detailed atom-by-atom structure of several key proteins involved in sensing DNA damage and repairing it, including p53, RecA, BRCA2, and others.
2000–2009: Expanding Cancer Research
Dr. Marks ended his 19-year tenure as MSK president in 1999. The person who succeeded him, Harold Varmus, had received a Nobel Prize in 1989 for his co-discovery, with J. Michael Bishop, of the cellular origin of viral oncogenes. A preeminent scientist and an accomplished administrator who had previously led the National Institutes of Health, Dr. Varmus was a natural choice to grow the stature and quality of research at SKI.
Dr. Varmus redoubled the institute’s commitment to the pursuit of scientific research, growing the number of programs and faculty in SKI. In 2002, he appointed Thomas Kelly to be SKI director. Dr. Kelly had overseen the creation of a world-class molecular biology program at Johns Hopkins University, and Dr. Varmus recognized him as a keen spotter of talent as well as a capable administrator.
Among the individuals Dr. Kelly recruited was immunologist James Allison, who arrived at SKI in 2004 and became chair of Immunology. In his previous position, at the University of California, Berkeley, Dr. Allison had discovered that a molecule called CTLA-4 acts as a brake or checkpoint on immune cells, restraining them from attacking. Releasing this brake with an antibody, he found, could cure cancer in mice. This work led eventually to the development of the first immune checkpoint inhibitor, ipilimumab. Dr. Allison’s decision to come to SKI was influenced by the opportunity to work closely with clinical researchers to shepherd his laboratory findings through the drug development pipeline all the way to patients.
“It’s a great example of how basic knowledge — in this case about how immune cells function — can lead to major new cancer breakthroughs,” Dr. Kelly says.

Immunologist James Allison developed the immunotherapy approach called checkpoint blockade.

Developmental biologist Kathryn Anderson discovered the role of cilia in cell signaling.

Molecular biologist Thomas Kelly led SKI from 2002 to 2013.
In addition to recruiting new talent, Dr. Kelly also reorganized the institute’s structure, first by dividing up the Molecular Biology Program.
“Molecular Biology was a funny program at that time,” says developmental biologist Kathryn Anderson, who arrived at SKI in 1996. “It was sort of half nucleic acids biochemistry and half development biology. It was an unusual marriage of these two very different interest groups.”
In 2002, Dr. Kelly split molecular biology and development into separate programs and assigned new leadership. Dr. Anderson became chair of Developmental Biology, while Ken Marians, an expert in DNA replication, remained chair of Molecular Biology.
Dr. Kelly also split Structural Biology off from Cell Biology, and created a new program in Cancer Biology and Genetics. Dr. Massagué, who had been chair of Cell Biology, was named the inaugural chair of this innovative new program that sought to bridge experimental and clinical aspects of cancer research. Alan Hall, who discovered the function of Rho GTPases in controlling the actin cytoskeleton, was brought in to lead Cell Biology in 2006.
Dr. Kelly was also influential in starting the Gerstner Sloan Kettering Graduate School of Biomedical Sciences (GSK). Although SKI had been involved in education since 1950, when it began allowing students from Cornell University Graduate School of Medical Sciences to conduct their research in SKI labs under the guidance of SKI faculty, it did not have a school of its own. GSK would take advantage of what was unique about the educational opportunity of SKI, namely the close collaboration between scientists and clinicians. GSK admitted its first class of students in 2006.
2010–today: Science to and from the Clinic
When Craig Thompson became president and CEO of MSK in 2010, he sought to bring about even more fruitful collaborations between scientists and clinicians across the institution. “I want us to realize the full clinical potential of all the extraordinary research that goes on here,” Dr. Thompson said.
To help execute that plan, he appointed Dr. Massagué as director of SKI. Having chaired both the Cell Biology Program and the Cancer Biology and Genetics Program, Dr. Massagué had a proven track record of leadership. He also shared Dr. Thompson’s belief in the power of collaboration between scientists and clinical researchers. Together, they worked to strengthen the research capabilities and collaborative opportunities across MSK.
Dr. Massagué established new programs in Chemical Biology and Computational & Systems Biology, and new collaborative research centers — the Metastasis and Tumor Ecosystems Center and the Center for Epigenetics Research.
He also initiated projects that seek to take maximal advantage of discoveries emerging from the clinic to bolster research into the principles of biology. The Functional Genomics Initiative, for example, brings findings about drug responsiveness — who responds and who doesn’t — back to researchers in SKI. They can then work out the molecular basis for these clinical results.
“SKI is the preeminent entity for basic, preclinical, and postclinical research in cancer science,” Dr. Massagué says.
Once considered too complicated to study, human biology has become a main focus of researchers in the institute. The ability to sequence human DNA and to analyze human tumor tissue with advanced microscopy techniques have allowed researchers to draw direct links between findings in mice and other model organisms to human cancers. Increasingly, SKI researchers are tapping what Dr. Massagué calls “the awesome power of the human as a model organism.”
Computational biologist Christina Leslie applies computer learning to big-data problems in biology.
Developmental biologist Lorenz Studer is using stem cells to treat Parkinson's disease.

Chemical biologist Yael David studies epigenetic mechanisms of gene regulation.
Immunologist Alexander Rudensky is a world expert on regulatory T cells.
An emerging focus of the institute is the study of epigenetics — chemical modifications to DNA and chromatin that affect gene regulation. Investigators from several different SKI programs work in this area, which has ramped up in recent years.
SKI is also expanding computational biology and its application of single-cell analysis to the study of cellular and genetic complexity of developing tissues and tumors.
The role of the immune system — both innate and adaptive — in restraining and shaping cancer development continues to be a strong focus of research at SKI. Researchers explore the biology of inflammation, natural killer cells, and the role of regulatory T cells in health and disease, among other topics.
The biology of metastasis, the role of the microbiome in health and disease, and the biology and applications of stem cells are all active areas of research. Scientists are even returning to the study of cancer metabolism, thanks to insights and discoveries made by Dr. Thompson, also a member of the Cancer Biology and Genetics Program.
Though much has changed at SKI since 1945, the underlying philosophy of the institute remains the same. “Although many investigators pursue research with an eye toward having an impact in the clinic,” Dr. Massagué says, “investigators must be free to pursue whatever their instinct tells them will provide the most penetrating insights into the unknown.”
Read more about recent discoveries and advances emerging from the Sloan Kettering Institute.