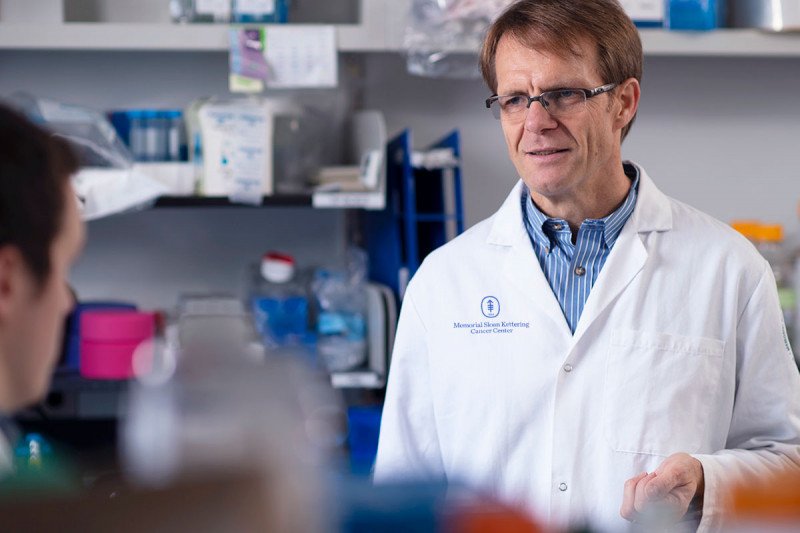
MSK developmental biologist Lorenz Studer
Memorial Sloan Kettering developmental biologist and Parkinson’s disease expert Lorenz Studer has been awarded an $8.95 million grant from the Aligning Science Across Parkinson’s (ASAP) Initiative, in partnership with the Michael J. Fox Foundation. Five institutions will share the award, with MSK being the lead grant recipient.
In an interview in September 2020, Dr. Studer spoke about what he hopes he and his fellow investigators can accomplish with this generous support.
Was the ASAP award something you applied for or were you surprised to receive it?
It was something we applied for. Initially, it was not on the top of my mind that I would apply for a grant focused on mechanistic biology, since the focus of my research in recent years has been more translational. But I discussed it with some of my colleagues, and it seemed to be really a unique opportunity.
In last 50 years, very little progress has been made in Parkinson’s disease, which results from the death of dopamine-producing neurons in the brain. The main treatment is still a drug called L-DOPA, which was first used in the 1960s and was revolutionary at the time. But it is not a cure, and eventually it stops working. I think the reason we haven’t made much progress is that we don’t really understand why these dopamine-producing cells die. And so maybe we need to take one step back and look at some fundamental questions about biology. It’s highly unusual that an organization like ASAP would invest so much money into the basic mechanisms, so we realized that this is an opportunity that doesn’t come along too often.
What will your lab specifically be studying?
One major part of what we will be doing here at the Sloan Kettering Institute is looking at aging as it is related to Parkinson’s disease. I’ve always been fascinated by the idea of what age means for a cell. For example, if we were to create induced stem cells from you now, as an adult, they would actually behave like an embryonic-stage version of your cells, and then they would age chronologically. So, if you wait nine months, your cells are going to be up to the stage of a newborn baby. They go all the way through the whole process. We are fascinated by that because it means that you can, to some extent, reset the age of the cell.
The question then becomes: Can you also make those cells 80 years old? Can you make an 80-year-old version of your brain with those cells? Many neurodegenerative diseases are age-related — Parkinson’s being an excellent example. Typically, a person is 60 to 70 years old when the disease begins. No baby gets Parkinson’s. Even in the very severe genetic form, people get it in their 30s or 40s. So then what is that age component, and how does it affect your genetic risk for disease as reflected in your DNA? Your DNA doesn’t change that much as you age. At 60 years, you have the same DNA, but something else happens that makes the disease develop.
Do you have the ability to artificially speed up the aging process in those cells?
That’s something we’ve been working on for a long time. One trick we have is to insert an aging-related gene into stem cells. You may have heard about these kids with a disease called progeria, which causes premature aging. When they are five or six years old they have wrinkled skin and look elderly. We can take the form of the gene that causes progeria in children and put it in stem cells and turn it on for a short period of time. In that way, we kind of fast-forward the movie of aging. It’s not perfect, but it definitely is something we are testing.
We also have some new ideas that we haven’t published data on yet, which come from a large grant from the National Institutes of Health. One strategy involves fiddling around with certain ways proteins are modified.
There are other research groups that are part of this grant. What are they studying?
We are looking at aging but will be working closely with the other groups. One team at Harvard is primarily interested in genetics, in particular looking at interactions between genes that might explain why one person who has a Parkinson’s risk gene gets the disease, while the other person with the same risk gene doesn’t.
Another group, at the New York Stem Cell Foundation, is working on cell interactions. So even though Parkinson’s disease is caused by the death of dopamine-producing neurons, maybe that’s not the only cell type that is involved. Maybe other cells contribute as well. For example, maybe they create an inflammatory environment that contributes to the death of these cells.
Two groups will collaborate on the computational part. They are using machine learning to take this massive amount of age data, genetic data, and cell data and then integrate it to make network models. They will try to see the ways that all these things interact. Are there nodes that stand out? These are possibly the most critical points. And they could perhaps be our future targets for treatment.
The coolest thing about this consortium is that we have different approaches, but also kind of similar ideas. So each of us have some ideas how each of those factors could contribute, but then we develop a way to understand very large numbers of age-related factors, very large numbers of gene-gene interactions, and very large numbers of cell interactions in an unbiased fashion. It’s a nice way to do that at a scale that really couldn’t be done before we had all these disciplines and people.
Moreover, the main thrust of everything in this project is human stem cells. Nothing is done in a mouse or in a zebrafish. It’s all done in human cells, which also has never been tried before.
So even after 50 years of research, we still don’t know why the dopamine producing cells die?
To some extent that’s true. There are hypotheses. One idea is that it’s a problem with the energy machinery of the cells, called the mitochondria. It turns out that these dopamine-producing cells are gigantic cells. If you think about the brain, you have about a hundred billion nerve cells. But you have only about half a million dopamine cells. They are a rare cell type, but their size is huge. Scientists recently tried to track how big one dopamine-producing nerve cell is. If you add up all the extensions of a single cell, it’s several meters. It’s one of the largest cells you can have in the body.
Each cell has about two to ten million connections, or synapses, with other nerve cells. So it’s a monster. And all of that is driven by one cell and the DNA of one nucleus. You can imagine that it takes a lot of energy to power these cells. Whenever you make energy, you also make byproducts called oxygen radicals that can damage the cells. So these cells might be particularly prone to this kind of damage. There is a lot of evidence to support this hypothesis.
Another main hypothesis is related to the cell’s “trash collection” system. Again, there is a lot of waste being produced in a very large cell. It has to be transported to the right place, but there’s also a limiting factor in how much waste can be produced in a timely manner. If they can’t handle all the waste, then certain factors such as damaged proteins can accumulate that can make the cells sick.
What are some aspects of Parkinson’s disease that people might not know about?
One aspect that often surprises people is that loss of smell is often an early precursor of Parkinson’s disease. If your sense of smell is very good and you can smell your wine, then you can be pretty confident that you’re not going to develop Parkinson’s any time soon. It’s not a hundred percent, but it’s a pretty good predictor.
Another main predictor is constipation. Many people who eventually develop Parkinson’s have complained about constipation way before they developed typical Parkinson’s symptoms. And that makes some sense. In your gut, you essentially have another nervous system, the enteric nervous system, which is sometimes called the second brain. It’s nearly 500 million cells. And some of those seem to die off even earlier than the dopamine cells in the brain. We don’t really know why yet, but it is a very interesting question.
You’ve been developing a stem cell-based treatment for Parkinson’s disease. What is the status of that?
We hope to have final approval from the US Food and Drug Administration by the end of this year to start our clinical trial. We’re just submitting all the documents that were requested. We already have patients who we think might be interested in the therapy, but the actual trial will probably start early next year.
It’s been a long journey to get to this point. First was developing a product that works well enough. And then, because it’s such a new therapy, there are a lot of regulatory issues to work out. Nobody has put large numbers of nerves cells into the brains of people before.
It took us nearly two years longer than we had planned, but we hope now is finally the moment where we can get the green light. The goal is to have a study of ten people.
You were awarded a MacArthur “Genius Grant” a few years back. What does your family think about that?
I don’t think they think about it too much. Usually it only comes up if I do something really dumb. “You are really a genius,” they’ll say. Both my son and daughter are actually much smarter than me. For example, my son is now a junior at MIT studying computer science, and he does all this sophisticated programming. If it takes me longer to figure something out compared to him, I’ll hear that joke, unfortunately.