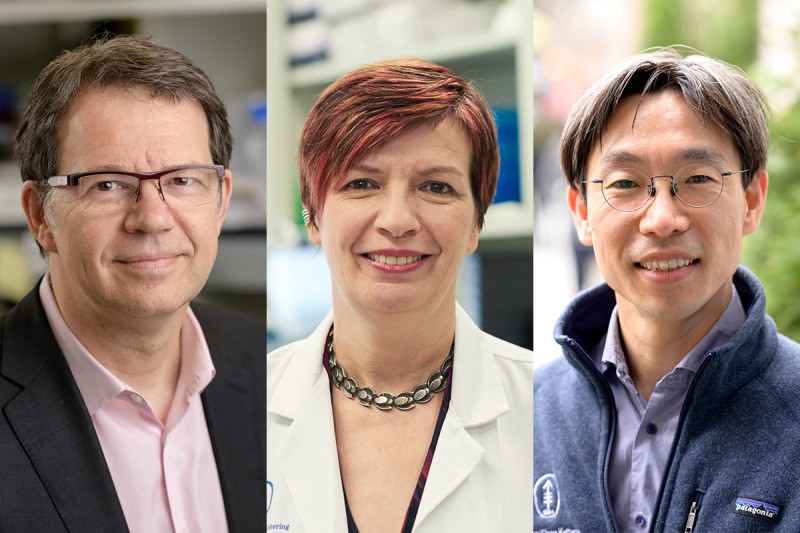
Dr. Michel Sadelain (left) and Dr. Isabelle Rivière (center) have pioneered many CAR T cell advances. The latest is the creation of CAR T cells using CRISPR, which are being tested in a clinical trial led by Dr. Jae Park (right).
CAR T cell therapy, often referred to as a “living drug,” has successfully treated blood cancers such as leukemia and lymphoma. The approach, which was pioneered at Memorial Sloan Kettering Cancer Center (MSK), involves equipping a person’s own immune cells (called T cells) with special receptors that can find cancer in the body and launch an immune attack against it.
To make the therapy even more precise and powerful, a clinical trial is now starting at MSK testing CAR T cells that were made using a genome-editing tool called CRISPR/Cas9.
This latest advance was made possible by the work of Michel Sadelain, MD, PhD, Director of the Center for Cell Engineering and the Gene Transfer and Gene Expression Laboratory at MSK, in collaboration with Isabelle Rivière, PhD, Director of MSK’s Cell Therapy and Cell Engineering Facility.
The clinical trial, led by hematologic oncologist Jae Park, MD, has the potential to change the future of immunotherapy.
The Advantages of CAR T Cells Created Using CRISPR
CRISPR allows researchers to precisely target and modify specific genes within the T cell genome, which makes the CAR T cells work better. In 2017, Dr. Sadelain reported in Nature that using CRISPR to insert the gene at a specific location made CAR T cells more effective at killing human tumor cells in a mouse model of leukemia.
“Many immunotherapies have been hampered because the T cells attack the cancer cells at first, only to become worn out — a phenomenon called T cell exhaustion,” he says. “The CRISPR CAR T cells seem to be more resilient and able to continue fighting cancer cells for longer periods.”
“Previously, CAR T cells had been made using a modified virus to deliver the CAR [chimeric antigen receptor] to the immune cells,” Dr. Rivière explains. “This method inserts the CAR at any location in the genome of the T cells. The somewhat scattershot approach can cause unwanted side effects. CRISPR allows for a more targeted delivery.”
In the 2017 study, Dr. Sadelain’s team showed it is possible to snip open the DNA at a precise location called TRAC. Because of the precise positioning of the inserted CAR at that chromosomal location, the engineered cells can turn the CAR on and off more easily. In conventional CAR T cells, the CAR is “on” all the time, which can cause the cells to start out strong but then quickly lose power. The CRISPR CAR T cells seem to conserve their power and last longer.
Under Dr. Rivière’s leadership, the Cell Therapy and Cell Engineering team at MSK has perfected the method of creating these cells to make them suitable for clinical use.
Using CRISPR CAR T Cells To Treat Diffuse Large B Cell Lymphoma
The phase 1 clinical trial led by Dr. Park uses the CRISPR-edited CAR T cells to treat diffuse large B cell lymphoma, the most common type of non-Hodgkin lymphoma. The CAR T cells target a protein on the surface of the cancer cells called CD19.
“We gave the T cells an additional boost by inserting a molecule called 1XX in the CAR and introducing it in the TRAC location,” Dr Rivière says. “This makes the cells more effective and prolongs their potency.”
“The trial will test three different doses of CRISPR CAR T cells to see what is the lowest dose that is both effective and safe,” Dr. Park says. The trial will enroll around 20 patients and is expected to take about two years.
MSK is currently conducting a phase 1 trial for the same disease, also led by Dr. Park. That trial is testing CAR T cells that target CD19 and include the 1XX molecule but were made in the conventional way, using a modified virus. The interim phase 1 results were reported in December 2022 at the annual meeting of the American Society of Hematology.
“Results showed the approach to be safe and very effective, with relatively low doses of CAR T cells, which is extremely encouraging,” Dr. Park says. “We can use that first trial to guide us in the new CRISPR trial so we can move on to the next phase.”
Reducing the Dose of CAR T Cells
The researchers hope the clinical trial will show that the CRISPR CAR T cells are better at eradicating the cancer the patient has and also make it possible to decrease the number of cells needed per injection.
“If the cells last longer, we ultimately would need fewer of them, which will make manufacturing easier,” Dr. Rivière says. “In addition, if the CRISPR cells persist longer, they may be able to find cancer cells that may have not been killed right after the infusion and may reemerge later. Establishing the CRISPR technology for cell engineering at MSK will open many more possibilities.”
Using CRISPR for Allogeneic, “Off-the-Shelf” Therapy From Healthy Donors
If the CRISPR approach works in patients, it could be a launchpad for using donated T cells — rather than a patient’s own T cells — because it could help reduce a common side effect in allogeneic treatments: preventing the transplanted donor cells from attacking the patient’s normal cells. This reaction is called graft-versus-host disease (GVHD), which can cause problems in the gastrointestinal tract, eyes, skin, liver, and other tissues.
“The precision of CRISPR can disable the part of the T cell that triggers GVHD,” Dr. Rivière says. “In addition, an allogeneic treatment from a readily available bank of healthy donor T cells could speed up the time needed to create a therapy because patients would not need to have CAR T cells made from their own cells. That process can take a month or more, although at MSK it’s been reduced to two to three weeks.”
Early this year, MSK reported encouraging results from allogeneic CAR T cells — created through conventional methods — to treat multiple myeloma. Several companies and academic teams are working on allogeneic CRISPR CAR T cells.
“One drawback so far seems to be that they don’t work as long compared with CAR T cells made from the patient’s own cells,” Dr. Sadelain says. “This challenge warrants further investigation.”
MSK’s History of Developing New CAR T Cell Treatments
MSK was the first institution to infuse CD19 CAR T cells into a patient with chronic lymphocytic leukemia in 2007 — eight years after Dr. Sadelain began establishing the cell engineering and manufacturing facility at MSK with Dr. Rivière as its director. The strong program built around MSK’s Center for Cell Engineering enabled MSK to:
- Design novel CAR T cells.
- Identify new targets, such as CD19 and GPRC5D.
- Introduce new features in CARs, such as 1XX.
- Use CRISPR/Cas9 technology to conduct cutting-edge clinical trials.
“The Cell Therapy and Cell Engineering Facility has been a unique laboratory that powers MSK research into the clinic,” Dr. Rivière says. “This has resulted in achieving several world-first advances in cell therapy over the years. The combination of innovative science with compassionate care for patients has placed MSK at the forefront of using these living drugs to fight cancer.”