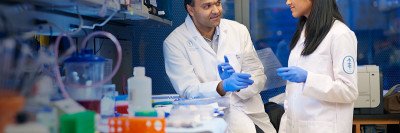
MSK cancer researchers Elizabeth Adams, Charles Sawyers, and Rohit Bose are studying the underlying biology of prostate cancer tumors in order to develop better treatments.
Prostate cancer is not one disease but many, defined by distinct classes of genomic changes. That is the message emerging from gene-sequencing projects like The Cancer Genome Atlas, which sought to map the mutational landscape of the most common cancers.
One clear group of people identified in this analysis is men with mutations in a gene called FOXA1. About 12% of men with prostate cancer have a detectable FOXA1 mutation. (The actual number may be much higher when other, less apparent versions are considered.) Men with FOXA1 mutations in their tumor have a worse prognosis than men without these mutations.
How changes in this gene lead to cancer is currently unknown. But a new study led by physician-scientist Charles Sawyers, who directs the Human Oncology and Pathogenesis Program at MSK, provides the first clues.
In experiments done in mouse prostate organoids, Dr. Sawyers and his team, including postdoctoral fellow Elizabeth Adams, showed that the most common FOXA1 mutations produce a version of the protein that is unusually effective at opening up regions of chromatin. Chromatin is the combination of DNA and proteins that makes up chromosomes. Tightly packed chromatin must be loosened so that genes can be expressed, or turned on, in a cell.
The investigators suspect that the changes in gene expression associated with these open regions contribute to cancer development.
“When we began the work, there was confusion about whether the alterations in FOXA1 were oncogenic drivers or loss-of-function tumor suppressor mutations,” Dr. Sawyers says. “It’s absolutely clear now that FOXA1 is an oncogene, not a tumor suppressor.” Oncogenes make proteins that promote cancer, while tumor suppressors are proteins that protect against cancer.
The findings were published on June 26 in the journal Nature.
A ‘Pioneering’ Study
FOXA1 is what’s known as a pioneer transcription factor, which means it comes along first and makes it possible for other transcription factors to act. It does this by binding directly to closed chromatin and opening it. Typical transcription factors cannot open chromatin.
FOXA1’s pioneering role may help explain how it can function effectively as a cancer promoter. It facilitates the expression of many genes at once. Moreover, mutations in different regions of the FOXA1 protein cause it to bind to and open different regions of chromatin, which leads to the turning on of unique subsets of genes.
“We went into this thinking that likely all of the FOXA1 mutations would behave in the same way,” says Dr. Adams, who is now a scientist at Constellation Pharmaceuticals in Boston. “But then some of them turned out to be driving a different differentiation pattern, so that was a bit of a surprise to us.”
Whether the FOXA1 oncogene is sufficient by itself to cause prostate cancer is not yet known, but there are hints that it may be.
“This is clearly a subtype of prostate cancer, which we knew very little about before this paper,” Dr. Sawyers says. “Now we have the first important clues about what’s driving it. I think this paper will vault FOXA1 to high on the list of possible targets for a drug company to consider.”
About Prostate Cancer
Prostate cancer is the most common cancer among men in the United States (not including non-melanoma skin cancer). It is more common in men older than 50. Depending on the tumor’s genetic makeup, the aggressiveness can vary greatly. Most men die with prostate cancer but not from it.