The immune system can clearly recognize cancer cells as different, yet often it is unable to stop them from growing. Scientists are trying to understand why.
It’s a mystery how a growing tumor escapes destruction by the immune system. Our immune cells are typically very good at recognizing altered or foreign cells and swiftly dispatching them. But in the case of a tumor, they seem to turn a blind eye.
New research from scientists at Memorial Sloan Kettering offers a clue about why that happens. In a paper published on November 30 in the journal eLife, a team led by David Scheinberg reported a startling discovery about the molecular features of cancer cells that the immune system recognizes as foreign. Suspicious-looking protein fragments, called neoantigens, stud a cancer cell’s surface. Roving immune cells called T cells can latch on to these neoantigens when they pass by.
Previously, scientists thought the only thing that mattered for a successful immune response against a cancer cell was how immunogenic its neoantigens are — essentially how suspicious they look to a patrolling immune cell. But the new research suggests that the abundance of neoantigens matters too.
“Unexpectedly, we found that the immune system could not destroy cells expressing even highly immunogenic neoantigens when they were found at low abundance,” says Ron Gejman, an MD/PhD student in the Scheinberg lab and the paper’s first author. “Somehow, these clearly altered cells are being missed.”
He says that the results help explain why cancer cells that the immune system theoretically could kill ultimately manage to escape destruction. The findings might even point to why tumors form in the first place.
A Powerful Antigen-Presenting Tool
The team made their discoveries using a tool called PresentER, which Dr. Gejman pioneered. It allows scientists to engineer an individual cell with a specific neoantigen on its surface. They can create thousands of such cells, each displaying a different neoantigen. Then they can inject mice with these cells and see which cells are destroyed by the animals’ immune system.
“We know very little about which neoantigens are recognized by the immune system,” says Dr. Scheinberg, Chair of the Molecular Pharmacology Program in the Sloan Kettering Institute and Director of the Center for Experimental Therapeutics at MSK. “When we started this work, it was to learn what makes a good neoantigen when it comes to eliciting an immune response.”
In general, cells that have “good,” or immunogenic, antigens will be detected by immune cells and destroyed. Those that have “bad,” or nonimmunogenic, antigens will not be detected and will be spared.
Unsurprisingly, the team found that when an immunogenic antigen was present on most or all of the cells in a tumor, the tumor was destroyed. But something different happened when they started to vary the number of unique antigens that they introduced into the mice, as well as the proportions of cells carrying each antigen.
When cells with an immunogenic antigen were present at about 10% of the total number of cells, the tumors could still be killed. But when the proportion of cells with an immunogenic antigen was less than 1% of the total, the tumor wasn’t killed. “It was still there three weeks later,” Dr. Gejman says.
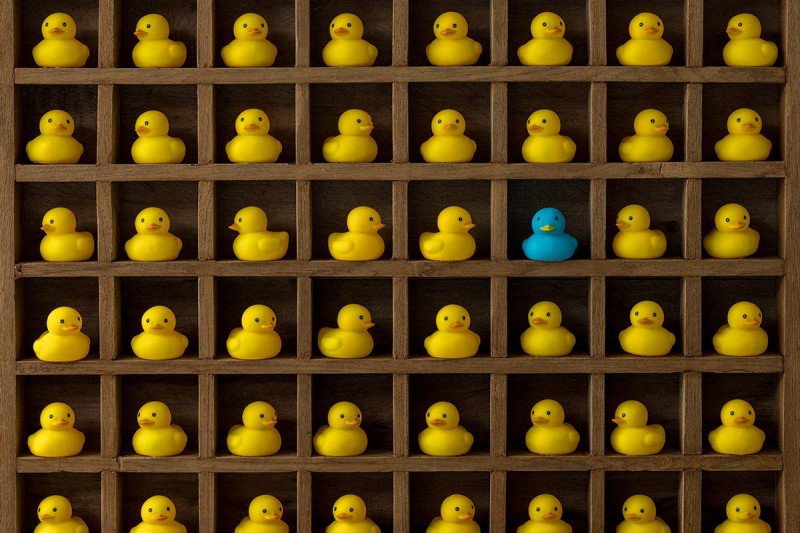
The scientists aren’t sure why the proportion of cells bearing a particular neoantigen — what they call the clonal fraction — matters. But they do have some ideas. One is that when a neoantigen is present at a low frequency in a tumor, T cells aren’t activated and prompted to look for cells displaying it. Another idea is that the T cells are in fact activated but can’t find their target amidst a sea of irrelevant antigens.
“You can imagine it’s like looking through a forest trying to find a single tree,” Dr. Gejman says. “Maybe they just can’t find it.”
Later, when these small collections of mutated tumor cells grow bigger, it is too late for the immune system to do much about them.
An Attention-Grabbing Result
The paper published on a Friday night and quickly garnered attention on social media, particularly Twitter. Dr. Gejman thinks that’s because the findings come at a time when doctors and researchers alike are trying to sort out some puzzling observations related to mutations and the immune system.
Many noncancerous cells — those in skin that has been exposed to UV light, for example — contain a slew of mutations and presumably plenty of neoantigens. Yet there is no evidence that the immune system typically prunes them.
Similarly, tumors often contain immune cells that recognize neoantigens found within them, yet the tumors are still able to grow.
And people with very heterogeneous tumors — with many different clones of cells — tend to benefit less from immunotherapy drugs than people with tumors that are more homogenous.
According to the investigators, these situations may come about because the clonal fraction of cells with immunogenic antigens is too low to generate an effective immune response. The researchers hope that by understanding more about why these cells go unnoticed, they can design immunotherapies that work for more people, and even perhaps nip growing cancers in the bud.



