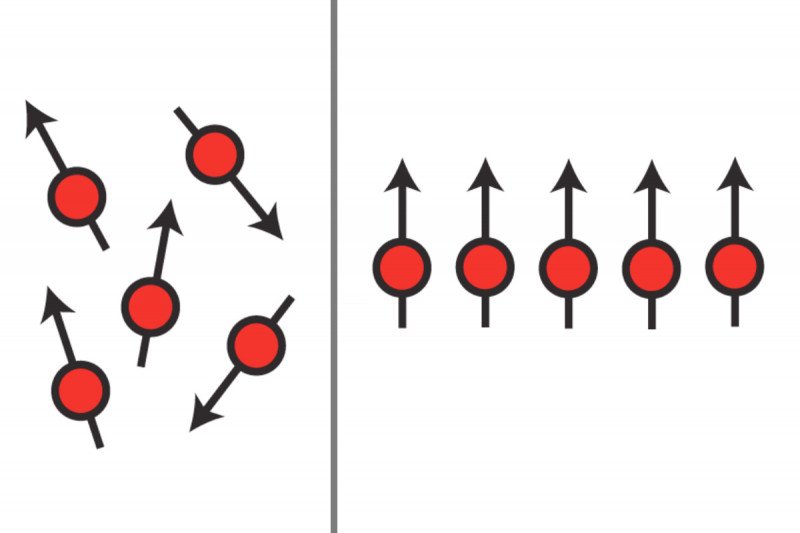
By strongly orienting molecules to an MRI’s magnetic field, hyperpolarization enhances what doctors can see and conclude about a treatment’s effect on a tumor.
Many people with cancer begin a treatment regimen hoping, but not knowing for certain, that the approach will work for them. Unfortunately, it can take weeks or even longer for doctors to determine whether a treatment is having the desired effect, and valuable time is often lost for patients who require another tactic.
A noninvasive imaging technology called hyperpolarized magnetic resonance imaging (MRI) may hold the key to shortening this initial period of uncertainty.
“With hyperpolarized MRI, we may be able to tell in 24 to 48 hours – rather than weeks – if a treatment is working,” explains Memorial Sloan Kettering biochemist and imaging specialist Kayvan Keshari, who has been studying the technology for many years. “And if it’s not, we can change the approach right away.”
Delivering Key Data Quickly and Safely
Hyperpolarized MRI is based on the premise that cancer cells use and metabolize nutrients differently, and often at a faster rate, than normal cells do. Prior to the procedure, the molecules of a sugar solution are oriented to an MRI’s magnetic field at an extremely low temperature (hyperpolarized) so that the normally very weak signal emitted by the substance is much stronger.
The more than 10,000-fold jump in signal strength with hyperpolarized MRI is like turning a penny into a $100 bill, Dr. Keshari explains.
The patient then receives the solution via an injection, and as the body processes the substance, doctors get a quick snapshot of whether cells’ metabolic processes are indicative of cancer.
By comparing these data with imaging done before treatment began, doctors could use this information to decide whether to continue treatment or to try a new approach. The tool could also one day spare some patients from needing to have additional biopsies or other invasive procedures that assess treatment response.
MSK is the first institution to use the new platform from General Electric Healthcare — called the GE SpinLab system — in patients. Testing began in May of this year in men with prostate cancer, a disease for which there currently is no broadly accepted approach for assessing how aggressive or responsive a treatment is.
Urologic surgeons James Eastham and Vincent Laudone, proponents of the new technology, say the data that hyperpolarized MRI provides represent a big leap beyond the basic information about tumor structure and size that conventional imaging technologies such as traditional MRI and CT scans are able to show.
There are also plans to investigate the use of this technology in breast, brain, liver, kidney, and bone cancers, as well as in soft tissue sarcomas. Farther down the road, Dr. Keshari says, hyperpolarized MRI could also be used to reveal additional information about a tumor, including its stage, genotype, or how aggressive it is.
Other MSK experts involved in the study and helping to bring the technology to the bedside include radiologist Hedvig Hricak, radiochemist Jason Lewis, surgeons, engineers, pharmacists, and numerous others.






